Feature Blog Article
February 28th is Rare Disease Day!

Feature Blog Article

Autoimmune hepatitis is a disease in which the body’s own immune system attacks the liver and causes it to become inflamed. The disease is chronic, meaning it lasts many years. If untreated, it can lead to cirrhosis and liver failure.
There are two forms of this disease. Type 1, or classic, autoimmune hepatitis is the more common form. This is the form that mostly affects young women and is often associated with other autoimmune diseases. Type 2 autoimmune hepatitis is less common and generally affects girls between the ages of 2 and 14.
Your immune system normally attacks bacteria, viruses and other invading organisms. It is not supposed to attack your own cells; if it does, the response is called autoimmunity. In autoimmune hepatitis, your immune system attacks your liver cells, causing long-term inflammation and liver damage. Scientists don’t know why the body attacks itself in this way, although heredity and prior infections may play a role.
Often, the symptoms of autoimmune hepatitis are minor. When symptoms do occur, the most common are fatigue, abdominal discomfort, aching joints, itching, jaundice (yellowing of the skin and whites of the eyes), enlarged liver, nausea and spider angiomas (blood vessels) on the skin. Other symptoms may include dark urine, loss of appetite, pale stools and absence of menstruation. More severe complications can include ascites (fluid in the abdomen) and mental confusion. In 10%-20% of cases, autoimmune hepatitis may present with symptoms like an acute hepatitis.
Autoimmune hepatitis often occurs suddenly. Initially, you may feel like you have a mild case of the flu. To confirm a diagnosis of autoimmune hepatitis, your doctor will use blood tests and a liver biopsy, in which a sample of liver tissue is removed with a needle for examination in a laboratory.
The goal of treatment is to stop the body’s attack on itself by suppressing the immune system. This is accomplished with a medicine called prednisone, a type of steroid. Often times, a second drug, azathioprine (Imuran) is also used. Treatment starts with a high dose of prednisone. When symptoms improve, the dosage is lowered and azathioprine may be added. In most cases, autoimmune hepatitis can be controlled but not cured. That is why most patients will need to stay on the medicine for years, and sometimes for life. Unfortunately, long-term use of steroid can cause serious side effects including diabetes, osteoporosis, high blood pressure, glaucoma, weight gain and decreased resistance to infection. Other medications may be needed to control these side effects.
About 70 percent of people with autoimmune hepatitis are women, usually between the ages of 15 and 40. Many people with this disease also have other autoimmune diseases, including type 1 diabetes, thyroiditis (inflammation of the thyroid gland), ulcerative colitis (inflammation of the colon), vitiligo (patchy loss of skin pigmentation), or Sjogren’s syndrome (dry eyes and dry mouth).
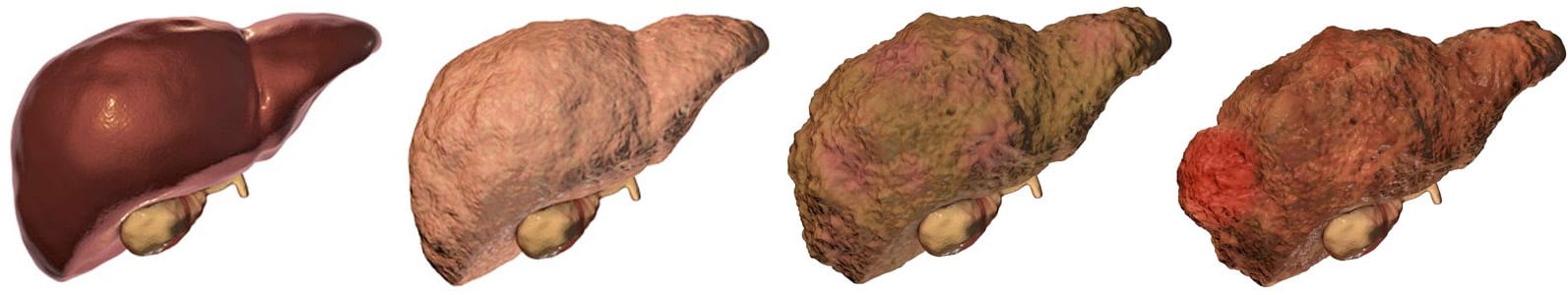
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on May 13, 2021