Feature Blog Article
Rare Liver Disease Summit Seeks to Improve Patient Health Outcomes

Feature Blog Article

Hemochromatosis is one of the most common genetic disorders in the United States. It is an inherited condition in which the body absorbs and stores too much iron. The extra iron builds up in several organs, especially the liver, and can cause serious damage. Without treatment, the disease can cause these organs to fail.
Iron is an essential nutrient found in many foods. Healthy people usually absorb about 10 percent of the iron contained in the food they eat to meet the body’s needs.
People with hemochromatosis absorb more than the body needs. The body has no natural way to rid itself of the excess iron, causing the excess to build up in the organs.
Many people have no symptoms, even in advanced cases. Joint pain is the most common complaint of people with hemochromatosis. Other common symptoms include fatigue, lack of energy, abdominal pain, loss of sex drive, and heart problems. Symptoms tend to occur in men between the ages of 30 and 50 and in women over age 50. However, many people have no symptoms when they are diagnosed.
If the disease is not detected early and treated, iron may accumulate in body tissues and may eventually lead to serious problems such as:
Genetic or hereditary hemochromatosis is connected to a defect in a gene called HFE, which regulates the amount of iron absorbed from food.
While hemochromatosis is present at birth, symptoms rarely appear before adulthood. A person who inherits the defective gene from both parents may develop hemochromatosis. A person who inherits the defective gene from only one parent is a carrier for the disease but usually does not develop it.
Juvenile hemochromatosis and neonatal hemochromatosis are two forms of the disease that are not caused by a HFE defect. Their cause is unknown. The juvenile form leads to severe iron overload and liver and heart disease in adolescents and young adults between the ages of 15 and 30, and the neonatal form causes the same problems in newborn infants.
Blood tests for serum iron and either total iron binding capacity or transferrin are good screening tests. A good additional test is serum ferritin level, which is elevated in patients with hemochromatosis. If these tests are persistently high, a genetic test for the mutations in the HFE gene should be performed.
Depending on whether there is evidence of liver damage, a liver biopsy should be done to assess the damage to the liver. Excess iron is also frequently present in patients with alcoholic liver disease or chronic viral hepatitis. A liver biopsy is the only definitive way to determine if patients with these diseases also have iron overload.
Treatment for hemochromatosis is simple, inexpensive, and safe. The first step is to rid the body of excess iron. The process is called phlebotomy, which means removing blood the same way it is drawn from donors at blood banks.
Depending on how severe the iron overload is, a pint of blood will be taken once or twice a week for several months to a year, and occasionally longer. The goal is to bring the iron levels in the blood to well within the normal range and keep them there.
Once iron levels return to normal, maintenance therapy, which involves giving a pint of blood every 2 to 4 months for life, begins. Some people may need it more often. An annual blood test will help determine how often blood should be removed.
People with hemochromatosis should not take iron supplements. Those who have liver damage should not drink alcoholic beverages because they may further damage the liver.
Immediate relatives of people with hemochromatosis should have their blood tested to see if they have the disease or are carriers, this includes parents, siblings and children.
Doctors should consider testing people who have joint disease, severe and continuing fatigue, heart disease, elevated liver enzymes, impotence, and diabetes, because these conditions may result from hemochromatosis.
People of Northern European descent are more prone to hemochromatosis than are people of other ethnic backgrounds. Men are five times as likely as women are to develop the condition, and they usually experience symptoms at an earlier age.
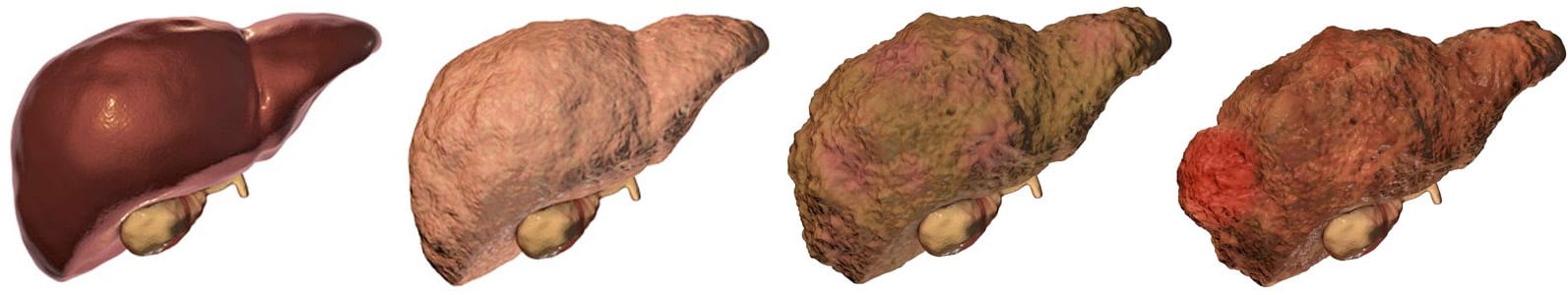
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on April 15, 2022