Feature Blog Article
Giving a Voice to the LGBTQ+ Community

Feature Blog Article

Hepatitis C is a disease caused by a virus that infects the liver. The virus, called the Hepatitis C virus or HCV for short, is just one of the hepatitis viruses. The other common hepatitis viruses are A and B, which differ somewhat from HCV in the way they are spread and treated. According to the Centers for Disease Control (CDC), an estimated 2.7 million people in the United States have chronic Hepatitis C infection. The CDC now recommends one-time hepatitis C testing of all adults (18 years and older) and all pregnant women during every pregnancy. CDC continues to recommend people with risk factors, including people who inject drugs, be tested regularly.
Explore this Hepatitis C Information Center by clicking through to the Diagnosis, Treatment and Support landing pages where you’ll find more information to help you manage Hepatitis C.
Explore options, learn the questions to ask, and find out what to expect during treatment.
What is hepatitis C?
Hepatitis C is a virus that affects the liver. It is the leading cause of liver failure and end stage liver disease and is a major cause of liver transplants in the United States.
When first infected, a person can develop an “acute” infection, which can range in severity from a very mild illness with few or no symptoms to a serious condition requiring hospitalization. Acute hepatitis C infection is a short-term illness that occurs within the first six months after someone is exposed to the hepatitis C virus. For most people, acute infection leads to chronic infection but for reasons that are not known, approximately 15% to 25% of people clear the virus without treatment.
Chronic hepatitis C infection is much more common. It can last a lifetime and lead to serious liver problems, including cirrhosis (scarring of the liver) or liver cancer.
How common is Hepatitis C in the United States?
An estimated 3.2 million Americans are infected with hepatitis C according to the Centers for Disease Control and Prevention (CDC), yet a whopping 75% are not aware that they carry the virus.
Each year, more than 17,000 Americans become infected. The CDC reports that 15,000 of people die from hepatitis C-related liver disease annually, surpassing the death rate from HIV.
Hepatitis C has been aptly called the silent epidemic. A person can have the virus for years – even decades — before they experience symptoms and by that time, liver damage has often occurred.
Who is most at risk?
Baby boomers are most at risk. So much so, that recently, New York Governor Andrew Cuomo signed legislation that will require hospitals and health service providers to offer testing for the virus to all patients born between 1945 and 1965. The law took effect on January 1, 2014.
How is Hepatitis C transmitted?
Hepatitis C is transmitted through direct blood-to-blood contact. It can be contracted and spread through blood transfusions (performed before 1992), unprotected sex, intravenous drug use with dirty or shared needles, body piercings and tattoos using non-sterile ink and needles, and sharing personal items such as toothbrushes, razors and nail clippers. It is not spread through exposure to sweat, urine or tears or close contact with an infected person who sneezes or coughs.
Can Hepatitis C be spread through sexual contact?
Yes, but to a lesser degree than with other forms of hepatitis such as hepatitis B but even a small risk of contracting hepatitis C, not to mention other sexually transmitted diseases, warrants protective and safe sexual practices.
Who should get tested?
Since universal screening of blood and blood products did not occur until 1992, anyone who had a blood transfusion or organ transplant before that time should be tested. It is recommended that people be tested for hepatitis C if they were/are:
What are the symptoms of Hepatitis C?
Most people initially have few or no symptoms for many years. When symptoms do emerge, they may present as fatigue, nausea, achiness, abdominal pain or flu-like symptoms.
Can Hepatitis C be cured?
Yes, you are considered cured if the hepatitis C virus is not detected when measured with a blood test three months after you’ve completed treatment. This is called a sustained virologic response (SVR) and data suggest that you will stay virus free indefinitely. And with newer drugs coming to market, cure rates of up to 90% have been seen in patients with hepatitis C.
Even more important sustained virologic response has been associated with lower rates of liver cancer, cirrhosis and all-cause mortality. This means that getting rid of hepatitis C allows individuals to live longer lives.
Will a person who has Hepatitis C ultimately need a liver transplant?
Undiagnosed and untreated hepatitis C can damage the liver to the point where a person could need a transplant. Not every person will develop advanced disease from hepatitis C.
But because we can’t always predict what will happen over time, the safest course for most people is to modify anything that can injure the liver before they have advanced disease. This includes curing the virus before there is extensive disease.
What is the difference between Hepatitis A, Hepatitis B and Hepatitis C?
Although they are all viruses that infect the liver, how you get them and how they can cause long-term health problems differ. Hepatitis A can be contracted through food or water that has been contaminated by fecal matter and raw shellfish. It does not lead to chronic disease and can be prevented through vaccinations. People generally recover within three to six weeks with no permanent liver damage.
Hepatitis B is also less common in the U.S. – affecting less than five percent of our population. It is spread through blood and body fluids, including saliva. There are also vaccines to prevent hepatitis B and newborns are vaccinated against this form of hepatitis before they even leave the hospital.
Unfortunately, there are no preventative vaccinations for hepatitis C, but early detection and advances in treatment can cure many strains of the disease.
Where can the public get more information?
The American Liver Foundation has a wealth of resources about preventing, screening/testing, treatment and living with hepatitis C, including a dedicated website hepc123.org, a national helpline – 1-800-GO-LIVER, on-line communities for people living with hepatitis C and a national database of liver specialists.
People don’t think about their livers as much as other organs but they should. Liver disease — and there are more than 100 types — is not something that just happens to alcoholics or drug users but some 30 million Americans, including children. Liver diseases have many causes including heredity, reactions to drugs or chemicals, lifestyle choices and viruses.
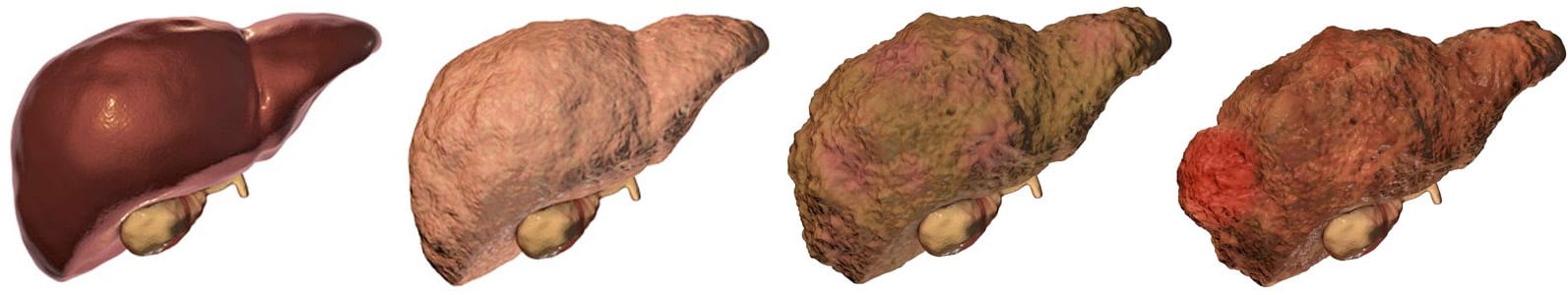
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on May 11, 2022