Feature Blog Article
NASH and the Roller-Coaster of Emotions

Feature Blog Article

Nonalcoholic fatty liver disease (NAFLD) is the build up of extra fat in liver cells that is not caused by alcohol. It is normal for the liver to contain some fat. However, if more than 5% – 10% percent of the liver’s weight is fat, then it is called a fatty liver (steatosis). The more severe form of NAFLD is called nonalcoholic steatohepatitis (NASH). NASH causes the liver to swell and become damaged.
Non-alcoholic fatty liver disease tends to develop in people who are overweight or obese or have diabetes, high cholesterol or high triglycerides. Rapid weight loss and poor eating habits also may lead to non-alcoholic fatty liver disease.
However, some people develop non-alcoholic fatty liver disease even if they do not have any risk factors. Non-alcoholic fatty liver disease affects up to 25% of people in the United States.
Read how Nick Giordano, a marathon runner, was diagnosed with non-alcoholic fatty liver disease.
Non-alcoholic fatty liver disease may cause the liver to swell (steatohepatitis). A swollen liver may cause scarring (cirrhosis) over time and may even lead to liver cancer or liver failure.
Non-alcoholic fatty liver disease often has no symptoms.
When symptoms occur, they may include fatigue, weakness, weight loss, loss of appetite, nausea, abdominal pain, spider-like blood vessels, yellowing of the skin and eyes (jaundice), itching, fluid build up and swelling of the legs (edema) and abdomen (ascites), and mental confusion.
Non-alcoholic fatty liver disease is initially suspected if blood tests show high levels of liver enzymes. However, other liver diseases are first ruled out through additional tests. Often, an ultrasound is used to confirm the Non-Alcoholic Fatty Liver Disease diagnosis.
There are no medical treatments yet for non-alcoholic fatty liver disease. Eating a healthy diet and exercising regularly may help prevent liver damage from starting or reverse it in the early stages.
There are ways to prevent non-alcoholic fatty liver disease:
NASH Support Group on Facebook
Visit the American Liver Foundation Nonalcoholic Steatohepatitis (NASH) support group on Facebook. For more details, click here…
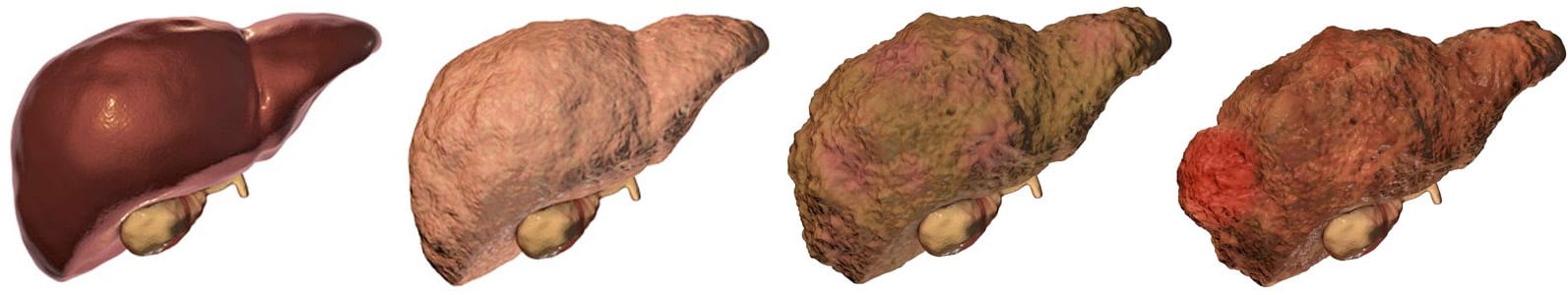
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on September 22, 2021