What causes biliary atresia?
The cause of this disease is not known. In some infants, the condition is most likely congenital, meaning present from birth. About one in 10 babies with biliary atresia have other congenital defects. Some research indicates that an early viral infection may be linked to biliary atresia.
Scientists do know that biliary atresia is not hereditary; parents do not pass it on to their child. It is also not contagious, and it is not preventable. It is also not caused by anything an expectant mother did or did not do.
What are the symptoms of biliary atresia?
Symptoms of biliary atresia usually appear between two and six weeks after birth. The baby will appear jaundiced, with yellowing of the skin and whites of the eyes. The liver may harden and the abdomen may become swollen. Stools appear pale grey and the urine may appear dark. Some babies may develop intense itching.
How is biliary atresia diagnosed?
Since other conditions lead to symptoms similar to those of biliary atresia, doctors must perform many tests before a conclusive diagnosis can be made. These tests may include blood and liver tests, an ultrasound examination, X-rays and a liver biopsy, in which a small amount of liver tissue is removed with a needle for examination in a laboratory.
How is biliary atresia treated?
Unfortunately, there is no cure for biliary atresia. The only treatment is a surgical procedure in which the blocked bile ducts outside the liver are replaced with a length of the baby’s own intestine, which acts as a new duct. This surgery is called the Kasai procedure after Dr. Morio Kasai, the Japanese surgeon who developed it.
The aim of the Kasai procedure is to allow drainage of bile from the liver into the intestine through the new duct. The operation is completely or partially successful about 80 percent of the time if performed early (before 3 months of age). In babies who respond well, jaundice and other symptoms usually disappear after several weeks.
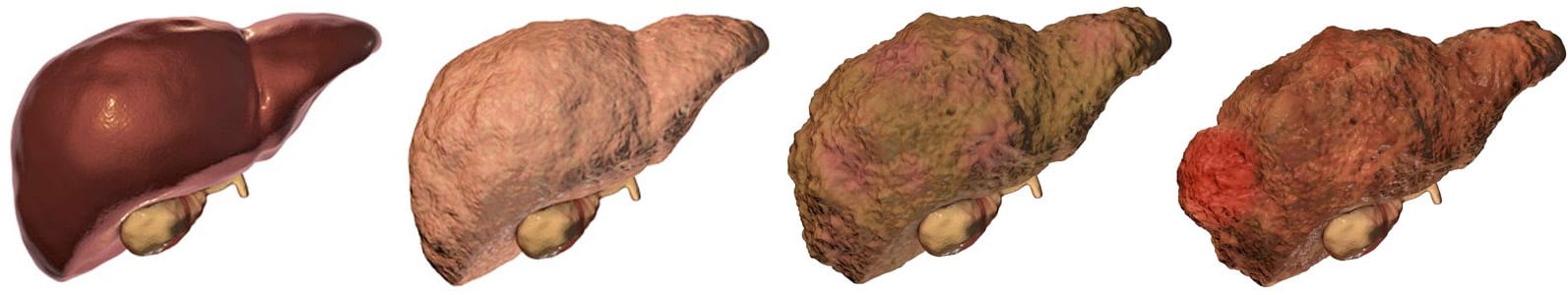
In cases where the Kasai procedure does not work, the problem often lies in the fact that blocked bile ducts are “intrahepatic,” or inside the liver, as well as extrahepatic, or outside the liver. No procedure, except for liver transplant, has been developed to replace blocked intrahepatic ducts.
The Kasai procedure is most successful in babies younger than 3-months-old, so early diagnosis is important.
If the Kasai procedure is not successful, the only other option is a liver transplant. However, a suitable donor organ must be found quickly, before damage to the liver from the backed-up bile becomes deadly.
What happens after surgery?
The aim of treatment after surgery is to encourage normal growth and development. If bile flow is good, the child is given a regular diet. If tests show that bile flow is reduced, a low-fat diet and vitamin supplements will be required, since the absorption of fats and vitamins is impaired.
What happens to children with biliary atresia?
Without successful treatment, few children with biliary atresia live beyond age two. In some cases, where the Kasai procedure is completely successful, the child may recover and live a normal life. However, in most cases, even when surgery is successful, patients will suffer gradual damage to the liver. These children will need specialized medical care throughout their lives, and many will ultimately need a liver transplant.