Feature Blog Article
Rare Liver Disease Summit Seeks to Improve Patient Health Outcomes
Type I glycogen storage disease (GSD I), also known as von Gierke’s disease, is the most common form of glycogen storage disease, accounting for 25% of all cases. It is an inherited disorder that affects the metabolism – the way the body breaks food down into energy.
After we eat, excess glucose is stored in the liver as glycogen to maintain normal glucose levels in our body. In GSD I, the enzyme needed to release glucose from glycogen is missing. When this occurs, a person cannot maintain his or her blood glucose levels and will develop hypoglycemia (low blood sugar) within a few hours after eating. The low levels of glucose in the blood of these individuals often result in chronic hunger, fatigue, and irritability. These symptoms are especially noticeable in infants.
Since people with GSD I are able to store glucose as glycogen but unable to release it normally, stores of glycogen build up in the liver over time and cause it to swell. The liver is able to perform many of its other functions normally, and there is no evidence of liver failure. The kidneys also become enlarged because of increased glycogen storage.
- Also known as von Gierke disease, is a more severe form of Glycogen Storage Disease.
- All Glycogen Storage diseases together affect fewer than 1 in 40,000 persons in the United States.
What are the symptoms of GSD I?
Children born with GSD I typically exhibit growth failure, chronic hunger, fatigue, irritability, an enlarged liver, and a swollen abdomen. Blood tests may indicate low blood sugar concentration and higher than normal levels of lipids and uric acid.
What causes GSD I?
GSD I is an inherited genetic disorder which causes the deficiency of one of the enzymes that work together to help the body break down the storage form of sugar (glycogen) into glucose, which the body uses to keep blood sugar stable when a person is not eating.
How is GSD I diagnosed?
Children with GSD I are usually diagnosed between 4 and 10 months of age. Testing will most likely include blood tests, imaging tests such as ultrasound to measure the liver and kidneys, and possibly a genetic test or liver biopsy.
How is GSD I treated?
The treatment of type I glycogen storage disease is focused on correcting the metabolic changes in the body and promoting the growth and development of the child. A combination of uncooked cornstarch mixed in water, soy formula, or soy milk is often recommended. Cornstarch is digested slowly, so it provides a steady release of glucose in between feedings.
Current treatments consist of providing small, frequent feedings during the day. Most doctors agree that certain sugars should be restricted, but the degree of restriction is still debated. In some cases, an overnight tube feeding, typically via a naso-gastric tube, is required to provide a continuous delivery of glucose.
Who is at risk for GSD I?
GSD I is an inherited genetic disorder. The effects of the disease are apparent very early in childhood.
- Do I have type 1 or type 2 GSD?
- How is GSD affecting my body?
- What is the treatment options for GSD?
- Are there specific foods or diet which would help my liver disease?
- Is my diagnosis of GSD genetic and if so, should others in my family be tested?
- Is my metabolism affected by GSD?
- If my metabolism is affected – are there medications or therapies which can help?
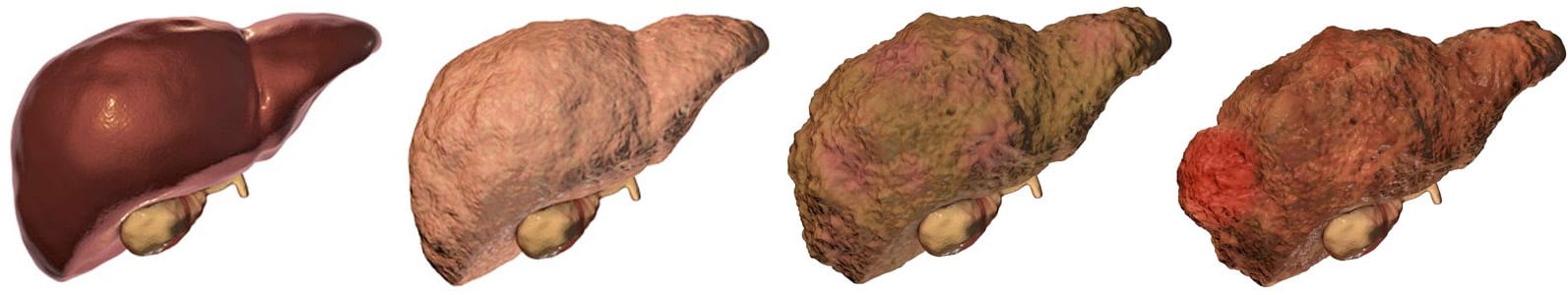
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on May 13, 2021
Share this page