Feature Blog Article
Reye syndrome is a rare illness that affects all bodily organs but is most harmful to the brain and the liver. It occurs primarily among children who are recovering from a viral infection, such as chicken pox or the flu. It usually develops a week after the onset of the viral illness but can also occur a few days after onset. Liver-related complications of Reye syndrome include fatty deposits, abnormal liver function tests, and poor blood clotting and bleeding caused by liver failure.
- Reye Syndrome is generally seen in children, most often between the ages of 6 to 12 years old.
- If the disease is found and treated early, most children recover from Reye Syndrome in a few weeks and have no lasting problems.
What are the symptoms of Reye Syndrome?
Reye syndrome is often misdiagnosed as encephalitis, meningitis, diabetes, drug overdose, poisoning, sudden infant death syndrome, or psychiatric illness.
Symptoms include persistent or recurrent vomiting, listlessness, personality changes such as irritability or combativeness, disorientation, delirium, convulsions, and loss of consciousness. If these symptoms are present during or soon after a viral illness, medical attention should be sought immediately. The symptoms of Reye syndrome in infants do not follow a typical pattern; for example, vomiting does not always occur. The onset of Reye syndrome can be rapid, and signs and symptoms may worsen within hours.
What causes Reye Syndrome?
The cause of Reye syndrome remains a mystery. However studies have shown that using aspirin to treat viral illnesses increases the risk of developing Reye syndrome. A physician should be consulted before giving a child any aspirin or anti-nausea medicines during a viral illness, which could hide the symptoms of the condition.
How is Reye Syndrome diagnosed?
If your child becomes sick with a possible case of Reye syndrome, doctors will want blood tests to evaluate his or her liver function. They may also evaluate other possible causes of liver problems and make sure your child does not have one of the rare inherited disorders that mimic Reye syndrome. In addition to blood and urine tests, diagnostic procedures may include spinal taps or liver biopsy.
How is Reye Syndrome treated?
There is no cure for Reye syndrome. Successful management, which relies on early diagnosis, is aimed primarily at protecting the brain from irreversible damage by reducing brain swelling, preventing complications in the lungs, and anticipating cardiac arrest.
Who is at risk for Reye Syndrome?
Reye syndrome occurs most commonly in children between the ages of 4 and 12, although it can occur at any age. It usually develops about a week after common viral infections such as influenza or chickenpox. Reye syndrome can also develop after an ordinary upper respiratory infection such as a cold. The precise reason is unknown, but using aspirin to treat a viral illness or infection may trigger the condition in children.
Reye syndrome may be a metabolic condition — one without symptoms (asymptomatic) — that is unmasked by viral illnesses.
What is the best way to prevent Reye Syndrome?
To reduce the risk of Reye syndrome, avoid giving aspirin or medications that contain aspirin to your child to treat viral illnesses. Other names for aspirin include: acetylsalicylic acid, acetylsalicylate, salicylic acid, and salicylate. Unless specifically instructed to do so by your child’s doctor, do not give aspirin to anyone younger than 19.
If your child or teenager has the flu or chickenpox, use other medications such as acetaminophen, ibuprofen, or naproxen sodium to reduce fever or relieve pain. Check the label on any medication to make sure it does not include aspirin before giving it your child, and be sure to give the correct dose.
- What are the most common problems to anticipate for my child?
- Are lethargy and confusion typical symptoms?
- Is my child likely to develop epilepsy as a result of this?
- Are there any medications which can be prescribed to help with vomiting and/or GI issues?
- For pain relievers in the future – which OTC would be safe for my child?
- What kind of follow up care will my child need?
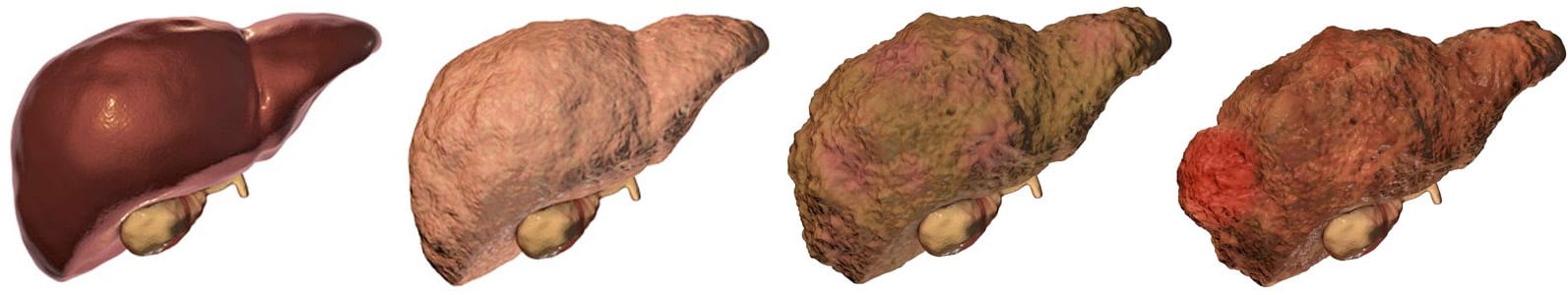
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on May 13, 2021
Share this page