Because HCV infection usually produces no symptoms or very mild symptoms during the early stages, many people don’t know they have it until liver damage shows up – sometimes decades later – during routine medical tests. Some people who get HCV have it for a short time (up to six months) and then get better on their own. This is called acute Hepatitis C. But most people (about 75% – 85%) will go on to develop chronic (or long-term) Hepatitis C, meaning it doesn’t go away.
Whereas Hepatitis A generally gives rise to acute hepatitis, Hepatitis C results in chronic hepatitis in most patients. An easy reminder is C for chronic in Hepatitis C and A for acute in Hepatitis A.
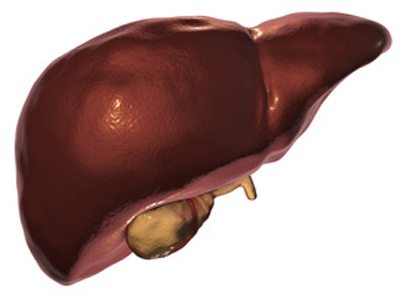
In order to understand your Hepatitis C infection, it helps to have a basic understanding of how your liver works. You only have one liver and it’s one of the largest and most important organs in your body. Your liver is located behind the lower right part of your ribs, which help protect it. Your liver does the following important jobs to keep you healthy:
- It acts like a filter to clean your blood by breaking down things such as alcohol, drugs (prescription, over-the counter and street drugs) and other harmful chemicals, and removes wastes.
- It stores nutrients that you need – such as vitamins, fat and sugar from food – as well as other chemicals, and releases them into your bloodstream when your body needs them.
- It produces some very important chemicals, like the ones needed to make your blood clot and heal after an injury, as well as a greenish fluid called bile that helps with the digestion of fats.
So what does all this have to do with Hepatitis C? Hepatitis means inflammation, or swelling, of the liver. When the liver is inflamed, it has a harder time doing its job. Hepatitis C is just one thing that can cause inflammation of the liver. Other things that can cause this include alcohol, some medications, and certain diseases.
Unless successfully treated with medication, chronic Hepatitis C infection can cause other serious health problems, such as cirrhosis, liver cancer and liver failure. However, with recent advances in Hepatitis C treatment we now have higher cure rates, shorter treatment times, and all-oral treatment regimens for most people. If you’re at risk for Hepatitis C, speak to your healthcare provider today about getting tested.
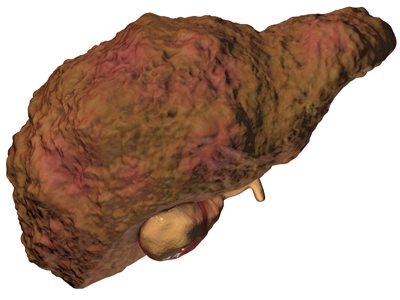
Cirrhosis
Fibrosis is the first stage of liver scarring. When scar tissue builds up and takes over most of the liver, this is a more serious problem called cirrhosis. Many people assume cirrhosis means liver disease from alcohol, but anything that damages your liver over many years can cause it to form scar tissue. As hard scar tissue replaces soft, healthy normal tissue the liver can no longer work well or work at all. It can take a long time – about 20 to 30 years – for liver damage to lead to cirrhosis.
In the early years, people with cirrhosis often have no symptoms. But over time, they can experience the following:
- tiredness
- weight loss
- nausea
- abdominal pain
- severe itching
- jaundice (yellow discoloration of the skin and eyes)
Eventually, people can have complications such as fluid in the abdomen and difficulty thinking clearly. We used to hear that cirrhosis could not be reversed, but research in a number of liver diseases – including Hepatitis C – found that scarring of the liver can be improved with treatment of the disease that initially led to the damage.
Liver Cancer
Like all organs in your body, your liver can get cancer. When this happens, some of the cells in your liver reproduce faster than they should, leading to tumors and other problems. People with Hepatitis C are at risk for liver cancer once they get to the level of cirrhosis. As such, it’s important for you to have some type of test to determine if you have cirrhosis. Remember that people with cirrhosis can feel fine and have no symptoms in the early stage.
Liver Failure
When someone has advanced liver disease and their liver is severely damaged it may no longer be able to function. The person may have yellow skin and eyes (jaundice), have fluid in their legs or abdomen (ascites), have bleeding from their stomach or esophagus (varices), or be confused (hepatic encephalopathy). At this point, a liver transplant may be considered.
Without treatment, chronic Hepatitis C can be very serious. But recent advances have made treatment shorter in duration, less difficult to tolerate and more effective. It’s an exciting and hopeful time for people with Hepatitis C as treatment is rapidly changing for the better.
Your risk of infection with HCV is increased if you:
- Shared needles to inject drugs or straws to inhale them
- Had tattoos or body piercings in an unclean environment using unsterile equipment
- Worked in a place where you came in contact with infected blood or needles, for example, healthcare workers
- Received a blood transfusion or organ transplant before July 1992
- Received a blood product for clotting problems made before 1987
- Needed to have your blood filtered by a machine (hemodialysis) for a long period of time because your kidneys weren’t working
- Were born to a mother with HCV
- Had unprotected sex with multiple partners
- Have or had a sexually transmitted disease
- Have HIV
Talk to your doctor about getting tested for Hepatitis C if you:
- Are a current or former drug user who used needles to inject, even if you only did this one time or did it many years ago
- Have a sex partner who has chronic Hepatitis C or have had many sex partners
- Had your blood filtered by a machine (hemodialysis) for a long period of time because your kidneys weren’t working
- Received a blood transfusion or organ transplant from a donor before July 1992
- Received a blood clotting factor to treat a bleeding disorder (like hemophilia) before 1987
- Are a healthcare worker and were exposed to blood through a needle stick or had other contact with blood or bodily fluids
- Have HIV
- Have evidence of liver disease, such as abnormal liver tests
- Were born between 1945 and 1965. The Centers for Disease Control and Prevention (CDC) recommends a one-time screening for all baby boomers.
Learn more, use the Centers for Disease Control’s Hepatitis Risk Assessment tool.
What the CDC Recommends
Were you born between 1945 and 1965? If so, then you’re a member of the Hepatitis C generation. The CDC (Center for Disease Control) recently recommended that all people born between during this time have a 1-time screening test for Hepatitis C. We now have new drugs that can treat and cure Hepatitis C so you should go get tested today.
Read the CDC Hepatitis C Fact Sheet
The life you save may be your own! Please contact your local healthcare provider.
Tests to Diagnose Hepatitis C
How is Hepatitis C diagnosed?
There are two main blood tests typically used to diagnose Hepatitis C. First, you’ll have a screening test that shows if you’ve ever had Hepatitis C at some point in your life. If this test is positive, you’ll have a second test to see if you have Hepatitis C now. These blood tests are described below:
Hepatitis C antibody test
This is the screening test used by doctors to show whether or not you have ever been exposed to Hepatitis C at some time in your life, by detecting antibodies in your blood. Antibodies are substances your body makes to fight off all kinds of infections. If you were ever infected with Hepatitis C, your body would have made antibodies to fight the virus.
If the test result is:
- Negative, it means you have not been exposed to Hepatitis C and further testing is usually not needed.
- Positive, you have had Hepatitis C at some point. However, it does not tell you whether you have it now. You’ll need to see your doctor for another test – the Hepatitis C RNA test – to determine if the virus is still active and present in your blood.
Hepatitis C RNA Qualitative Test
This test will determine whether or not you are currently infected with Hepatitis C. It is often called the PCR test because of the process used (polymerase chain reaction – hence PCR). It looks for the genetic material (RNA) of the Hepatitis C virus in your blood.
If the test result is:
- Positive, it is reported as “detected.” This confirms that you have Hepatitis C.
- Negative, it is reported as “not detected.” This means that even though you might have been exposed to the virus at some point, your body has cleared the infection on its own.
Hepatitis C RNA Quantitative Test
The quantitative test measures the amount of Hepatitis C virus present in your blood. This measurement is called the “viral load,” and is reported as an exact number.
This test is often used to monitor a person’s response to treatment for Hepatitis C by comparing the amount of virus in your bloodstream before, during, and after treatment. If you have lower levels of virus in your blood before starting treatment, you may have a better chance of getting rid of the virus.
Additional Tests You Might Need
Once you’ve been diagnosed with Hepatitis C, your doctor will likely order a number of tests to find out about the health of your liver and decide on a treatment plan that’s most appropriate for you.
Hepatitis C genotype
The Hepatitis C genotype refers to a specific “strain” or type of the Hepatitis C virus. There are six major types of Hepatitis C around the world: genotypes 1, 2, 3, 4, 5 and 6. In the United States, genotypes 1, 2, and 3 are common:
- Genotype 1: Most Americans (nearly 75%) with Hepatitis C have this type
- Genotype 2: About 10% of Americans with Hepatitis C have this type
- Genotype 3: About 6% of Americans with Hepatitis C have this type
The genotype of Hepatitis C does not change over time, so you only need to get tested once.
Genotype tests are done before a person starts treatment. Hepatitis C treatment works differently for different genotypes, so knowing your genotype helps your doctor choose the best treatment for you.
Testing for Hepatitis A and Hepatitis B
Your doctor may test to see if your body is immune to Hepatitis A and Hepatitis B. If these tests show no prior exposure or protection, he or she will recommend that you be vaccinated against these two viruses to eliminate the chance of becoming infected.
Liver function tests (LFTs) or liver enzymes
Now that you have Hepatitis C, your liver may not work as well. Liver function tests are a group of blood tests that detect inflammation and damage to the liver. They are used to detect, evaluate, and monitor liver disease and damage.
The cells in the liver contain proteins called enzymes, which are chemicals that help your liver do its work. When liver cells are damaged or destroyed, the enzymes in the cells leak out into the blood where they can be measured by blood tests. Liver enzyme testing usually checks the blood for two main enzymes:
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
Liver function tests also include ALP (alkaline phosphatase) and total bilirubin, among other things.
If your liver is damaged due to inflammation, enzymes pass out of your liver into your bloodstream making the levels of ALT and AST higher than normal. However, it’s common for people with chronic Hepatitis C to have liver enzyme levels that go up and down over time, sometimes returning to normal for as long as a year. So even if you have Hepatitis C, it’s possible for your liver enzyme tests to come back as normal.
The ALT and AST levels do not tell you how much scarring (fibrosis) there is in your liver and they do not predict how much liver damage will develop. However, if your total bilirubin is elevated, that could be a sign of cirrhosis (advanced scarring) and needs further investigation.
Tests to measure liver scarring or fibrosis
It’s important that you get some measure of the amount of scarring in your liver. This will guide your Hepatitis C treatment, as well as the long-term management of your liver health. Your Hepatitis C provider will make a recommendation for one of the following tests:
- Liver Biopsy
In order to determine whether the virus has caused scarring to your liver, your doctor may order a liver biopsy. During a biopsy, your doctor will insert a needle between your ribs into your liver to collect a small sample of liver tissue for laboratory testing.
- Elastography
Instead of a liver biopsy, some providers will test for liver stiffness by using a special ultrasound machine, the most common being FibroScan. The more scarring that is present in the liver the stiffer it is. This exam, called transient elastography is painless and non-invasive. If you are scheduled for this test, do not eat or drink for two hours beforehand.
- Serum markers
There are a number of blood tests available to estimate the amount of scarring in the liver.
Imaging tests
Your doctor may order tests that take images, or pictures, of your liver to make sure you do not have liver cancer. Different types of images can be obtained by using various types of equipment including ultrasound, a CT (computerized tomography) scan, or MRI (magnetic resonance imaging). If you have cirrhosis, these tests will be used to check for cancer as part of a screening program. Unless your Hepatitis C is very advanced, these tests will not tell you about your liver function or the overall health of your liver. Talk to your healthcare provider about why the test is being done.
Ask your doctor to explain all your test results and don’t hesitate to ask questions. This will help you have a better understanding of what’s happening in your body and why your healthcare provider is recommending a particular course of treatment.
Most people (about 70% – 80%) with an acute Hepatitis C infection do not experience any symptoms or show signs of the infection. If Hepatitis C symptoms do occur, they usually appear within two weeks to six months after being exposed to the Hepatitis C virus (HCV). If you do develop symptoms related to Hepatitis C, they’re generally mild and flu-like and may include:
- Feeling very tired
- Sore muscles
- Joint pain
- Fever
- Nausea or poor appetite
- Stomach pain
- Itchy skin
- Dark urine
- A yellow discoloration of the skin and whites of the eyes, called jaundice.
Since most people with acute Hepatitis C go on to develop chronic Hepatitis C – meaning the virus has remained in your body for 6 months or longer – and still have no Hep C symptoms, it’s common to have the infection for 15 years or longer before being diagnosed.
Watch HCV – The Silent Killer (video)
Hepatitis C is transmitted or spread when the blood from a Hepatitis C-infected person enters the bloodstream of someone who is not infected. Today, most people become infected with HCV by sharing needles or other equipment to inject drugs. Before 1992, when screening donated blood and organs for Hepatitis C was not standard in the United States, the disease was commonly spread through blood transfusions and organ transplants.
Hepatitis C can be transmitted through sex between a man and a woman, but the risk is low. Therefore, condoms are not routinely recommended for monogamous, heterosexual couples. The risk of Hepatitis C transmission is higher with unprotected anal sex between two men; using condoms will decrease this risk. All people with multiple sex partners should use condoms to reduce the risk of getting Hepatitis C and/or HIV.
Hepatitis C may be spread if there is a breakdown in the skin or lining of the mouth. Therefore, sharing of toothbrushes, razor blades and nail clippers is not recommended.
Is Hepatitis C contagious?
Hepatitis C transmission happens only through exposure to an infected person’s blood. It is not contagious like the common cold. You cannot get, or give, Hepatitis C by:
- Kissing
- Hugging
- Holding hands
- Casual contact
- Sneezing
- Coughing
- Sharing eating utensils
- Sharing food or drink
- Breastfeeding (unless nipples are cracked and bleeding)
There is no vaccine to prevent Hepatitis C, but there is research being done to develop one. Currently, vaccines are only available for Hepatitis A and Hepatitis B.
Remember that Hepatitis C is transmitted or spread when the blood from a Hepatitis C-infected person enters the bloodstream of someone who is not infected. If you don’t have Hepatitis C, you can reduce your risk of becoming infected by doing the following:
- If you’re injecting drugs, try to get into a treatment program. If you continue to use drugs, don’t share needles or other equipment with anyone else. Many cities have needle exchange programs that provide free, sterile needles.
- Make sure all equipment has been sterilized if you’re getting body piercings or a tattoo.
- If you’re a healthcare worker follow your institution’s safety precautions. For example, wear protective clothing and gloves and dispose of contaminated sharp objects properly.
- If you have more than one sex partner or are a man having sex with other men, use condoms for intercourse.
Watch The Stigma of HCV (video)
Hepatitis C can be spread through sexual intercourse, but the risk is considered to be low. It is extremely rare among monogamous couples, meaning couples who only have sex with one another. The risk increases if you:
- Have multiple sex partners
- Engage in rough sex
- Have a sexually transmitted disease
- Are infected with HIV
There is no evidence that Hepatitis C is spread by oral sex.
To reduce the chance of getting or giving Hepatitis C through sexual contact, follow these guidelines:
- Decrease the number of people you have sex with or have sex with only one person.
- Use latex condoms every time you have sex, particularly if you have:
- More than one partner
- Rough sex that might make one of you bleed
- Sex during your or your partner’s menstrual period
- Sex when you or your partner has an open sore on either of your genitals
When someone has both Hepatitis C and HIV, it is often referred to as HCV-HIV co-infection. This means that you have two infections in your body at the same time. HIV, the term for human immunodeficiency virus, is the virus that causes AIDS. You can find more detailed information about HIV and AIDS on several Web sties, including:
- Centers for Disease Control and Prevention
- United States Department of Veterans Affairs
- HIVandHepatitis.com
- The Body
HCV-HIV co-infection is fairly common. Overall, about one-third of all Americans infected with HIV also have Hepatitis C. And the rate of co-infection is much higher among injection drug users. More than half of people who have HIV and use injection drugs are also infected with Hepatitis C.
People that are co-infected can be effectively treated. However, since there are two infections to deal with managing them is more complicated. There is no cure for HIV, but it can be controlled. Hepatitis C can be treated successfully. Working closely with a doctor who specializes in managing co-infections will give you the best chance for successful treatment.
There are specific risks associated with co-infection. Having HIV, in addition to Hepatitis C, does the following:
- Quickens Hepatitis C disease progression
- Triples the risk for liver disease, liver failure and liver-related death
- Increases the chance that Hepatitis C will be sexually transmitted
- Increases the chance that a mother will infect her unborn child with Hepatitis C
Unlike Hepatitis A and Hepatitis B, a vaccine for Hepatitis C is not available.
However, treatment options are available and Hepatitis C may be cured (or cleared from the body).
Learn more about your treatment options and speak to your healthcare provider today.
The Hepatitis C virus is considered “cured” if the virus is not detected in your blood when measured with a blood test 3 months after treatment is completed. This is called a sustained virologic response (SVR) and data suggest that you will stay virus free indefinitely.
Try to keep yourself as healthy as possible, keep your medical appointments and get regular check-ups. Remember that you could become re-infected if you expose yourself to high-risk situations such as injection drug use, and so do everything possible to avoid these situations. Speak with a substance abuse counselor if needed.
Watch HCV: The Relief of a Cure (video)
Watch Hepatitis C Hidden Truths #3 “HOPE FOR A CURE” (video)
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Last Updated on March 10, 2020
Share this page