Feature Blog Article
Alpha-1 antitrypsin deficiency (Alpha-1) is a hereditary genetic disorder which may lead to the development of lung and/or liver disease. It is the most common genetic cause of liver disease in children. Adults can also be affected by Alpha-1 and may develop lung conditions such as emphysema as well as liver problems. Fortunately, many persons diagnosed with Alpha-1 never develop any of the associated diseases.
- This disorder affects about 1 in 1,500 to 3,500 individuals with European ancestry.
- Some people with Alpha-1 Antitrypsin Deficiency are misdiagnosed with asthma.
- Approximately 15% of adults with Alpha-1 Antitrypsin Deficiency develop liver damage (cirrhosis) due to the formation of scar tissue in the liver.
What are the symptoms of Alpha-1 Antitrypsin Deficiency?
In newborns, the typical symptoms of Alpha-1 are jaundice, swelling of the abdomen, and poor feeding. Alpha-1 may also appear in late childhood or adulthood and be detected because of fatigue, poor appetite, swelling of the abdomen and legs or abnormal liver tests.
What causes Alpha-1 Antitrypsin Deficiency?
Alpha-1 antitrypsin is a protein made in the liver which plays an important role in preventing the breakdown of enzymes in various organs. Individuals with Alpha-1 have a genetic disorder that prevents their body from creating enough of this protein. This trait must be inherited from both parents (who are, by definition, carriers) in order to cause the disorder.
How is Alpha-1 Antitrypsin Deficiency diagnosed?
The diagnosis of Alpha-1 is made by blood tests showing the low levels of alpha-1 antitrypsin and abnormal liver tests. Other tests such as ultrasound imaging or tests using specialized X-ray techniques may be necessary. A liver biopsy may be performed to check for damage to the liver.
How is Alpha-1 Antitrypsin Deficiency treated?
Currently, there is no cure for Alpha-1. Treatment is designed to maintain normal nutrition, to provide the liver and the body with essential nutrients, and to identify complications early in order to treat them better. Multiple vitamins and vitamins E, D, and K are often given. Certain abnormalities can be treated or controlled. Jaundice, severe itching, and fluid retention can all be dealt with through medication.
Who is at risk for Alpha-1 Antitrypsin Deficiency?
Worldwide, approximately 1 in 2,500 individuals has Alpha-1 Antitrypsin Deficiency. This disorder is found in all ethnic groups; however, it occurs most frequently in whites of European ancestry.
- Have you ever treated someone with this liver disease before?
- Since Alpha 1 is genetic, should my children be tested?
- Do I have liver damage?
- Will I need a liver transplant?
- Should I see a specialist to check my pulmonary functions?
- Should I see a specialist to check my cardiac health?
- Will I need augmentation therapy?
- What kinds of foods would best help my liver?
- Can you help me quit smoking?
- Are there any clinical trials available for my liver disease?
Alpha-1 Antitrypsin Deficiency Q&A Part 2
Alpha-1 Antitrypsin Deficiency Q&A Part 1
What is Alpha-1 Antitrypsin Deficiency?
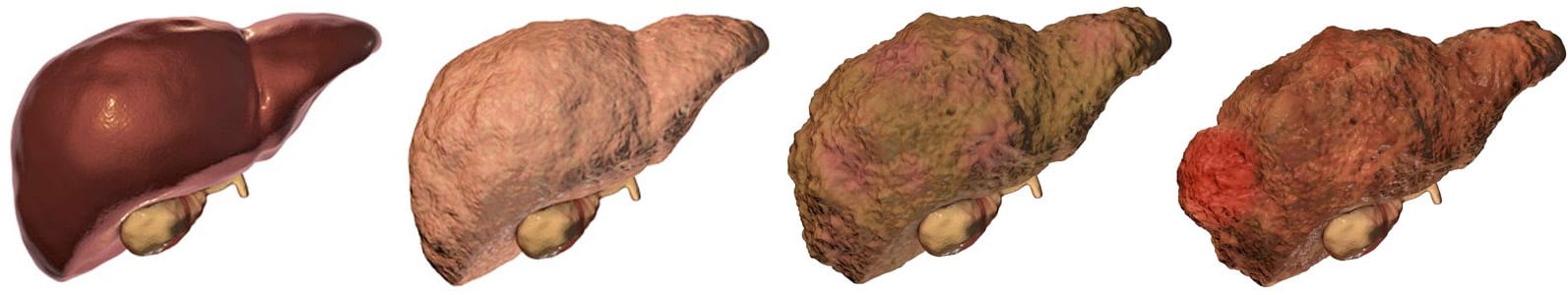
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on December 22, 2021
Share this page