Feature Blog Article
- Alcohol-related liver disease is caused by excessive consumption of alcohol.
- It is a common, but preventable, disease.
- Women are more likely to suffer liver damage from alcohol than men.
- Excessive alcohol consumption contributes to 3 types of liver disease…
- …fatty liver, where excess fat builds up in the liver…
- …alcoholic hepatitis, in which the liver cells become inflamed…
- …and alcohol-related cirrhosis, in which normal liver tissue is replaced by non-living scar tissue.
- Abstinence is the most important therapeutic intervention for people with this disease.
- In the early stages of the disease, liver damage may be reversed if the person stops drinking.
- Virtually all heavy drinkers develop fatty liver.
- Up to 35 percent develop alcoholic hepatitis and between 10 and 20 percent develop cirrhosis.
- Alcohol-related cirrhosis is the most serious form of alcohol-related liver disease.
- The damage from alcohol-related cirrhosis is not reversible and can cause fatal liver failure.
- Alcohol remains the second most common cause of liver cirrhosis after hepatitis C virus (HCV) infection in the United States, contributing to approximately 20% to 25% cases of liver cirrhosis.
What are the different types of alcohol-related liver disease?
Alcohol-related liver disease, as the name implies, is caused by excessive consumption of alcohol and is a common, but preventable, disease. For most people, moderate drinking will not lead to the disease. There are three main types of alcohol-related liver disease:
Fatty liver, also called steatosis, is the earliest stage of alcohol-related liver disease and the most common alcohol-related liver disorder. It is characterized by an excessive accumulation of fat inside liver cells, which makes it harder for the liver to function. Usually there are no symptoms, although the liver can be enlarged and you may experience upper abdominal discomfort on the right side. Fatty liver occurs fairly soon in almost all people who drink heavily. The condition will usually go away if you stop drinking.
Alcoholic hepatitis is an inflammation, or swelling, of the liver accompanied by the destruction of liver cells. Up to 35 percent of heavy drinkers develop alcoholic hepatitis, which can be mild or severe. Symptoms may include fever, jaundice, nausea, vomiting, abdominal pain and tenderness. In its mild form, alcoholic hepatitis can last for years and will cause progressive liver damage, although the damage may be reversible over time if you stop drinking. In its severe, acute form the disease may occur suddenly – after binge drinking for instance – and can quickly lead to life-threatening complications.
Alcohol-related cirrhosis is the most serious type of alcohol-related liver disease. Cirrhosis refers to the replacement of normal liver tissue with nonliving scar tissue. Between 10 and 20 percent of heavy drinkers develop cirrhosis, usually after 10 or more years of drinking. Anything that damages the liver over many years can lead the liver to form scar tissue. Fibrosis is the first stage of liver scarring. When scar tissue builds up and takes over most of the liver, it’s referred to as cirrhosis.
Symptoms of cirrhosis include those of alcoholic hepatitis, as well as the following:
- Accumulation of fluid in the abdomen (ascites)
- High blood pressure in the liver (portal hypertension)
- Bleeding from veins in the esophagus (esophageal varices)
- Behavior changes and confusion
- Enlarged spleen
Research has shown that cirrhosis can be reversed, although this may not occur for all patients. Cirrhosis caused by alcohol can be a life-threatening disease.
How does alcohol affect the liver?
Drinking too much alcohol, either on a single occasion – known as binge drinking – or drinking a lot over time, can take a serious toll on your health and well-being. In addition to injuring the liver, alcohol has many effects on your body including:
- Lessening your ability to think clearly and move with coordination; it can change your mood and behavior.
- Disrupting the processes involved in digestion, leading to malnutrition and weight loss.
- Weakening your immune system and the ability to fight infections. Increasing your risk of developing certain cancers including cancers of the colon, liver, esophagus, mouth, and breast (for women).
Is there a safe level of drinking?
 For most people, moderate drinking will not lead to alcohol-related liver disease. According to the Dietary Guidelines for Americans, moderate drinking is one drink a day for women and two drinks a day for men. Each of these alcoholic beverages, in the following amounts, is considered one drink and contains the same amount of alcohol:
For most people, moderate drinking will not lead to alcohol-related liver disease. According to the Dietary Guidelines for Americans, moderate drinking is one drink a day for women and two drinks a day for men. Each of these alcoholic beverages, in the following amounts, is considered one drink and contains the same amount of alcohol:
- One 12-ounce bottle of beer
- One 4-ounce glass of wine
- One 1-ounce shot of hard liquor.
However, if you have chronic liver disease, even small amounts of alcohol can make your liver disease worse. People with alcohol-related liver disease and those with cirrhosis from any cause should abstain from alcohol completely.
What factors increase your risk for alcohol-related liver disease?
The amount of alcohol you consume is the most important risk factor for developing alcohol-related liver disease. The risk increases with the length of time and amount of alcohol you drink. However, because many people who drink heavily or binge drink do not develop alcohol-related liver disease, we know there are other factors that affect a person’s susceptibility. Additional risk factors that play a role in someone developing alcohol-related liver disease include:
Obesity: Obesity is a contributing factor to fatty liver disease. The combined effect of obesity and alcohol together is worse than the effect of either one of them alone.
Malnutrition: Many people who drink heavily are malnourished, either because they eat poorly due to loss of appetite and nausea or because alcohol and its toxic byproducts prevent the body from breaking down and absorbing nutrients. In both cases, the lack of nutrients contributes to liver cell damage.
Genetic factors: Genetics can influence how the body processes alcohol and may predispose someone to alcoholism and alcohol-related liver disease.
Race and ethnicity: A higher risk of liver injury appears to be associated with one’s racial and ethnic heritage. For example, rates of alcoholic cirrhosis are higher in African-American and Hispanic males compared with Caucasian males.
Your gender: Women are more susceptible than men to the adverse effects of alcohol. Pattern of drinking: It’s worse to drink outside of meal times and binge drink, defined as five drinks for men and four drinks for women in one sitting.
Chronic viral hepatitis, particularly hepatitis C: The combined effect of alcohol and viral hepatitis on the liver results in more advanced disease than either of them alone.
How does alcohol-related liver disease progress?
Many heavy drinkers will progress from fatty liver disease to alcoholic hepatitis to alcoholic cirrhosis over time. However, some heavy drinkers may develop cirrhosis without first having alcoholic hepatitis first. Others may have alcoholic hepatitis but never have symptoms. Additionally, alcohol consumption may worsen liver injury caused by non-alcohol-related liver diseases such as chronic hepatitis C.
Since an individual’s susceptibility to the toxic effects of alcohol may vary by many factors including age, gender, genetics and coexistent medical conditions, it is reasonable for you to review alcohol use with your physician.
What are the complications of alcohol-related liver disease?
Complications from alcohol-related liver disease usually occur after years of heavy drinking. These complications can be serious.
They may include liver related conditions that are a consequence of portal hypertension:
- build up of fluid in the abdomen
- bleeding from veins in the esophagus or stomach
- enlarged spleen
- brain disorders and coma
- kidney failure
- liver cancer
In addition alcoholic liver disease may be accompanied by multi-organ non-liver conditions.
How is alcohol-related liver disease diagnosed?
Alcohol-related liver disease may be suspected based on a person’s history of alcohol abuse, laboratory or radiologic abnormalities or medical conditions related to alcohol abuse. Blood tests may be used to rule out other liver diseases. Your doctor also may need to do a liver biopsy. During a biopsy, a small piece of liver tissue is removed and studied in the lab.
How is alcohol-related liver disease treated?
Abstinence: If you’ve been diagnosed with alcohol-related liver disease, the single most important thing you can do for yourself is to stop drinking. Abstinence is the only way of possibly reversing liver damage, or in more advanced cases, preventing it from becoming worse. Discuss treatment options with your healthcare provider; these can include counseling, medications, an outpatient treatment program or a residential inpatient stay. If you are physically addicted to alcohol, medical supervision in a detoxification (or detox) program may be required to safely reduce your alcohol levels. It can be dangerous to stop drinking very suddenly. A rapid reduction in alcohol can lead to withdrawal symptoms including anxiety, agitation, hallucinations and seizures. Your doctor can recommend a program that best meets your needs.
Nutrition therapy: Nutritional deficiencies are very common in people with alcohol-related liver disease. Your doctor will likely recommend a special diet, as well as vitamin and nutritional supplements, to combat the effects of malnutrition and help you gain weight if needed. You may be referred to a nutritionist who can assist you with meal planning. If you have trouble eating enough to get the vitamins and nutrients you need, your doctor may recommend giving you a special nutrient-rich liquid intravenously or via tube feeding.
Medications: Depending on the severity of your disease, your doctor may recommend medications to help reduce liver inflammation. These drugs have shown some short-term benefit in increasing survival. Steroid treatment with prednisolone is usually the first-line medication, followed by pentoxifylline, if steroid therapy doesn’t work. No alternative medicine treatments have been found to cure alcoholic hepatitis.
Liver transplant: For people with advanced alcoholic cirrhosis, the only treatment option may be a liver transplant. However, active alcoholics do not usually qualify as suitable organ recipients. For transplant to be an option, you’d need to find a transplant center that would consider you and then meet the requirements of the program, including abstaining from alcohol for six months prior to transplant and agreeing not to resume drinking afterward.
What is the outlook for people with alcohol-related liver disease?
Anyone with alcohol-related liver disease will improve their health and life expectancy if they stop drinking. People with fatty liver may be able to use alcohol moderately after their liver recovers. People with alcoholic hepatitis or alcoholic cirrhosis should stop drinking completely. For those people with alcohol-related liver disease who do not stop drinking the outlook is poor. They are likely to suffer a variety of life-threatening health problems caused by alcohol-related liver disease.
Where can I get help?
In order to recover from your liver disease, you must stay sober. Participating in a group, like Alcoholics Anonymous (AA), or attending individual and/or group counseling sessions can help you maintain your sobriety. The following organizations are good resources for information on alcoholism:
Alcoholics Anonymous
National Institute on Alcohol Abuse and Alcoholism
www.niaaa.nih.gov/alcohol-health
Substance Abuse and Mental Health Services Administration
- What is the status of my liver?
- Do I have liver damage?
- Are there medications I will need to reduce inflammation in my liver (if I have inflammation)?
- Will I need a liver transplant?
- If I need a liver transplant, do you know the hospital in my region’s policies regarding alcohol?
- Will I need imaging studies to examine at my liver i.e. ultrasound, CT, or MRI?
- Will I need to have an endoscopy to check for varices?
- What treatment facilities are available in my community?
- Are there any support groups I could also attend along with attending a treatment center?
- Would I benefit from reducing the quantity of my alcohol intake or would I need to stop all together?
- Should I seek out care to address mental dependences (anxiety, depression)?
- How often should I be following up with you?
- Will I need to do routine bloodwork (every months, 3 months, 6 months, or year?)
- Are there changes in my diet I should make?
- Are there lifestyle changes I should such as exercising?
- What kinds of exercising would be appropriate for me?
Ask the Experts Webinar: Updates in Management of Chronic Liver Disease
Alcohol-Related Liver Disease Webinar Presented by Julie Spivack, MD of Gastroenterology Associates
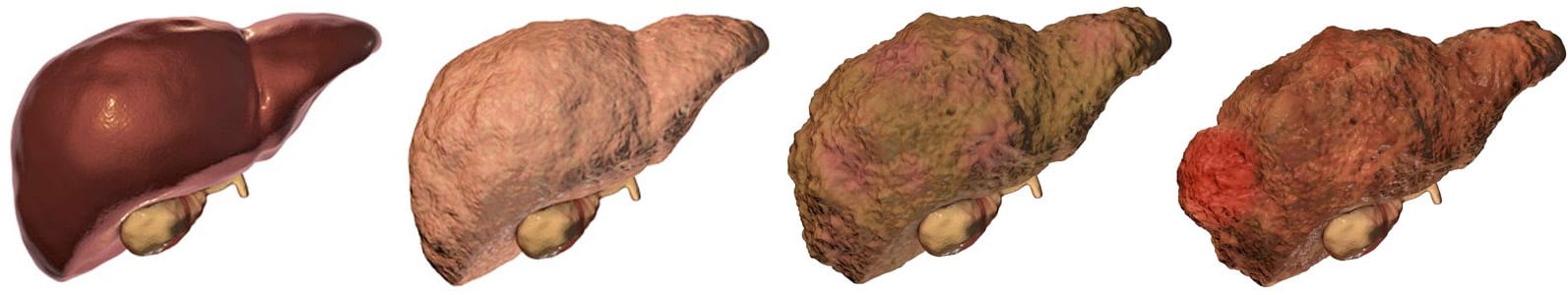
There are many different types of liver disease. But no matter what type you have, the damage to your liver is likely to progress in a similar way.
Whether your liver is infected with a virus, injured by chemicals, or under attack from your own immune system, the basic danger is the same – that your liver will become so damaged that it can no longer work to keep you alive.
Cirrhosis, liver cancer, and liver failure are serious conditions that can threaten your life. Once you have reached these stages of liver disease, your treatment options may be very limited.
That’s why it’s important to catch liver disease early, in the inflammation and fibrosis stages. If you are treated successfully at these stages, your liver may have a chance to heal itself and recover.
Talk to your doctor about liver disease. Find out if you are at risk or if you should undergo any tests or vaccinations.
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Last Updated on June 29, 2022
Share this page