In America, liver disease affects millions and is on the rise. Did you know there are more than 100 different types of liver disease? Living with long-term, chronic liver disease can cause damage to your liver.
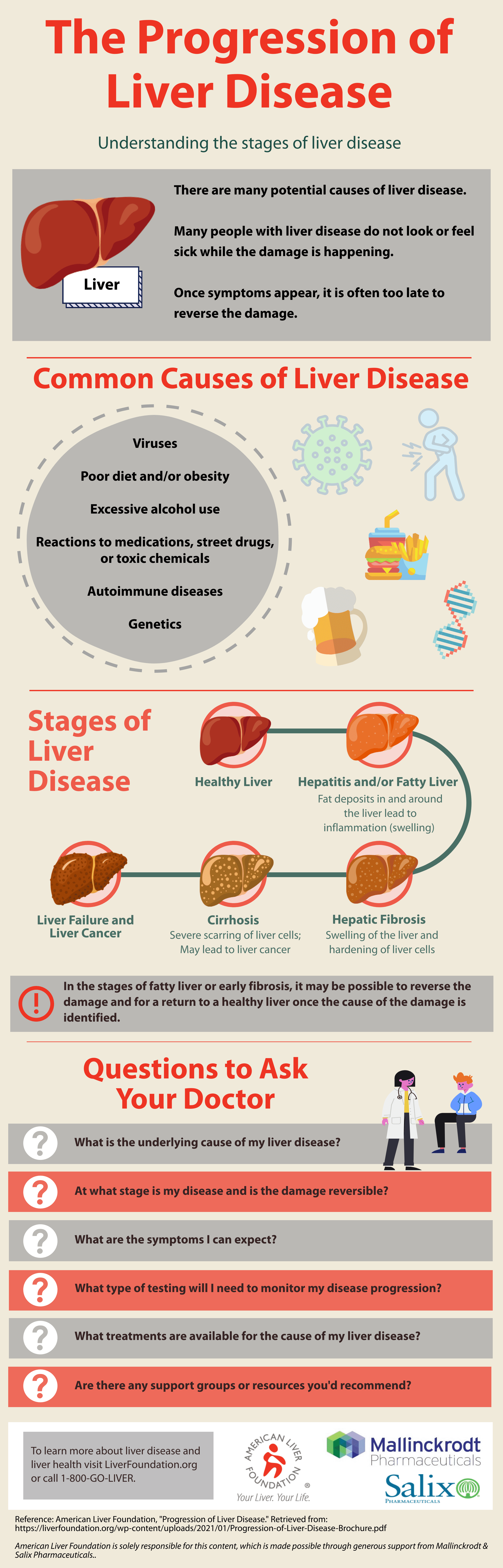
Common Causes of Liver Disease
- Viruses
- Genetics
- Autoimmune disease
- Excessive use of alcohol
- Poor diet and/or obesity
- Reactions to medications, street drugs, or toxic chemicals
Most liver diseases damage your liver in similar ways and for many, the progression of liver disease looks the same regardless of the underlying disease.
Early Diagnosis of Liver Disease is Very Important
Early diagnosis may prevent damage from occurring in your liver. Your liver is an incredible organ. If you’re diagnosed when some scar tissue has already formed, your liver can repair and even regenerate itself. Because of this, damage from liver disease can often be reversed with a well-managed treatment plan.
Many people with liver disease do not look or feel sick even though damage is happening to their liver. At a certain point in the progression of liver disease damage can become irreversible and lead to liver failure, liver cancer, or death.
We all need a healthy liver to live – it’s so essential that “live” is in the name!
Where to Find Your Liver
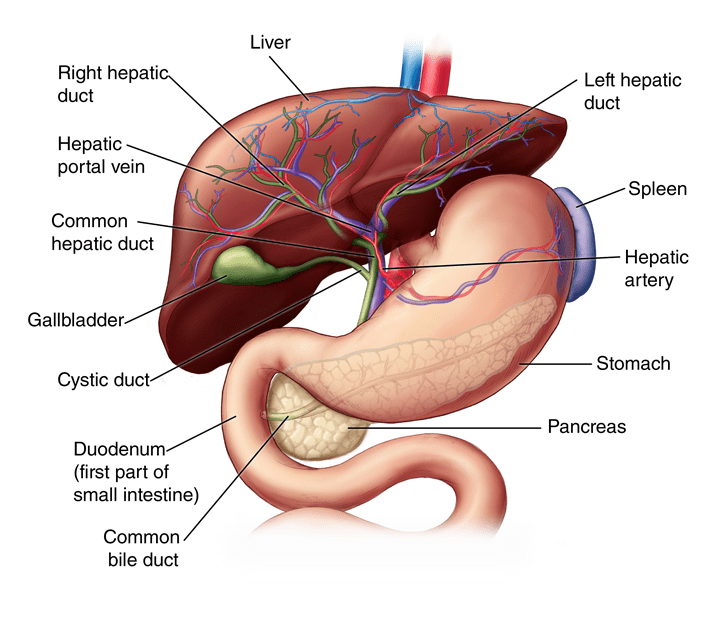
The liver is your body’s largest internal organ, weighing between 3 and 5 pounds. Your liver is located on the right side of your upper body, below the lungs, taking up most of the space in your rib cage. The gallbladder, which stores bile made in the liver, is found tucked under your liver. Your liver is made up of two separate sections, or lobes: the larger right lobe and the smaller left lobe. These two lobes are separated by tissue which anchors your liver in place.
 What Your Liver Does
What Your Liver Does
Your liver’s biggest role is to filter your blood all day, every day. A healthy liver gets its color, a deep reddish brown, because it is so drenched in blood. At any given moment, your liver contains about a pint of blood, or 13% of the body’s total blood supply. Your liver filters more than a liter of blood every minute which is about 22 gallons of blood per hour and more than 250 gallons of blood in a 24-hour time period. There are two sources that supply your liver with all that blood: the hepatic artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood to your liver. Blood coming from your digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
The Parts of Your Liver
As was mentioned earlier, the liver has two lobes. Each lobe is made up of smaller sections called lobules which are clusters of liver cells. The portal vein and the hepatic artery enter the liver sending one large trunk to the left lobe and one large trunk to the right lobe, gradually dividing into smaller branches creating a network of vessels bringing blood to each lobule. Once the cells in the lobule process the blood, ducts (small tubes) transport bile from the cell while filtered blood empties into veins at the center of each lobule. Veins lead out of the lobules merging into larger veins eventually flowing into the hepatic veins; blood then leaves the liver through the inferior vena cava, the largest vein in the body. Ducts transport bile out of the lobule flowing into larger right and left hepatic ducts. These two larger ducts come together to form the common hepatic duct. The common hepatic duct drains the bile to the gallbladder where it is stored and brings bile to the first part of the small intestine.
How Your Liver Works
Unlike the lungs or heart, we cannot feel our liver working. Many people don’t think about their liver unless or until there is something wrong with it. Your liver is an incredibly hard-working organ with more than 500 different vital functions. Only your brain has more functions than the liver. Many of the liver’s functions are related to your metabolism. These metabolic functions allow you to convert food to energy, break down food to basic building blocks needed by your body and eliminate waste.
The liver…
- Produces bile
- Bile is a yellow-green acidic liquid that helps carry away waste and break down fats in the small intestine during digestion
- Produces proteins for blood plasma
- Blood plasma is a fluid which transports blood components (red and white blood cells and platelets), nutrients, hormones, proteins, and waste products
- Produces cholesterol and special proteins to help carry fats through the body
- Converts unused glucose into glycogen for storage
- When needed, glycogen can be converted back to glucose for energy
- Balances blood sugar and makes glucose as needed
- Regulates levels of amino acids in blood
- Amino acids form the building blocks of proteins
- Stores iron processed from hemoglobin
- Hemoglobin is the protein in your red blood cells that carries oxygen
- Converts poisonous ammonia, made during digestion, to urea
- Processes drugs and other poisonous substances to your body
- Regulates blood clotting (or our ability to stop bleeding)
- Fights infections by making immune factors and removing bacteria from the bloodstream
- Removes bilirubin from red blood cells
The liver removes harmful substances from our body often by breaking them down to smaller byproducts. These byproducts leave the liver through bile or blood – byproducts in bile are removed from the body through feces while those in the blood are filtered out by the kidneys and removed through urine.
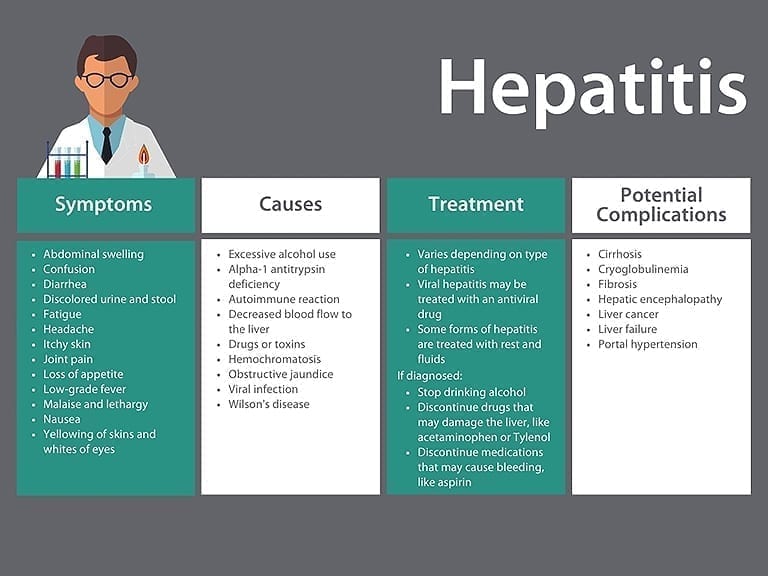
Did you know that hepatitis simply means inflammation of the liver?
Inflammation is the body’s natural response to injury and an important part of healing or immune response. Think about when you get a cut or injury to your skin. The area around the wound becomes swollen or inflamed. Seeing the swelling is not the only way you experience the inflammatory phase. You may also experience pain, redness, or the wound may feel warm to the touch. Under the skin, your body is hard at work to stop the bleeding and prevent infection. Blood vessels near the wound widen, or dilate, making more room for special healing and repair cells, or cells in the wounded area. These cells remove damaged cells and harmful substances (like bacteria or viruses) and allow the rest of the healing process to continue. Inflammation is essential to fight infection.
Inflammation’s Role in Metabolism
The liver is a complicated organ with many functions. The liver plays a big role in our immune system, making many important proteins needed for proper immune function. A lot of the liver’s functions are metabolic functions, related to our metabolism; these functions allow us to convert food to energy, break down food to basic building blocks needed by our body, and eliminate waste. Some of these metabolic functions require inflammation in order to occur. Similarly, the liver is responsible for filtering toxins, medications, and harmful substances from our blood. When the liver detects something dangerous it works hard to eliminate and clear the substance from our body. This activates an immune response which requires some inflammation. When the inflammation is no longer required there is a system in place to resolve the inflammation and keep the liver healthy.
Inflammation’s Role in Repairing Damaged Cells
The liver recognizes and replaces its own damaged or broken-down cells while still performing all of its vital functions. Just as inflammation is required to get rid of toxic substances, inflammation is part of repairing damaged liver cells. Damaged liver cells and immune cells both send out messages to activate specific repair cells which travel to the site of the injury. These repair cells release something called collagen, a fiber, which stiffens the tissue around the cells, protects the surviving cells and allows healing to occur. In a healthy liver, this repair process is very closely regulated and when no longer needed the extra collagen will disperse and the liver returns to normal.
When Inflammation Becomes Disease
While this controlled inflammation is essential to maintain proper function and balance in the liver, if it becomes dysregulated it drives the progression of liver disease. This diseased inflammation is called hepatitis. We most often hear the word hepatitis when we talk about viral hepatitis, like hepatitis A, B, or C, but viruses are not the only cause of hepatitis. Infection with a virus, overindulging in alcohol or fatty foods, or even our own immune system can trigger a continual inflammatory response in the liver, disrupting the closely regulated cycle of inflammation and healing. When someone has liver disease, their liver enters into a very dangerous cycle. Persistent inflammation sends nonstop signals to the repair cells to continue depositing collagen. The extra collagen stiffens around the tissue like it is supposed to in the healthy liver but, instead of a signal being released to stop the inflammation and discard the extra collagen, the inflammation continues and even more collagen is deposited leading to more stiffening. This is how scars or fibroids, develop in the liver. If left untreated, the scars will continue to replace healthy liver cells, leading to severe scarring known as cirrhosis.
It’s important to speak to your doctor about any possible risk factors for hepatitis or if you’ve experienced symptoms. There are many different causes for hepatitis with varying risks and symptoms. You can review possible symptoms and common causes of liver inflammation here in this infographic, explore more of this website or call the ALF Help Line 1-800-GO-LIVER to learn more.
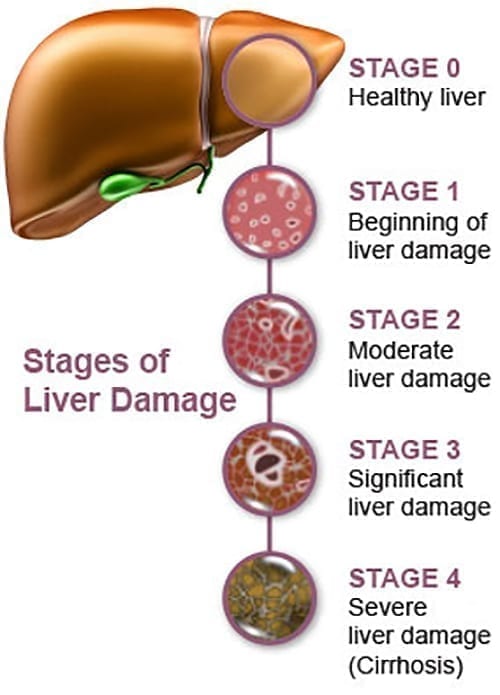
How Fibrosis Develops
When someone has liver disease, their liver enters into a very dangerous cycle. Persistent inflammation, or hepatitis, sends nonstop signals to repair cells to continue depositing collagen. The extra collagen stiffens around the tissue like it is supposed to in the healthy liver; but, instead of a signal being released to stop the inflammation and discard the extra collagen, the inflammation continues, and even more collagen is deposited, leading to more stiffening. This is how fibrosis develops.
When repetitive damage or long-lasting inflammation occurs, collagen and other proteins build-up between liver cells, forming scar tissue. Scar tissue can block or limit blood flow within the liver, starving and killing healthy liver cells, causing more scar tissue to form. Unlike healthy liver cells, scar tissue cannot function or repair itself. As fibrosis advances it can impact the liver’s ability to function, limit its ability repair itself and restrict blood flow. Over time, the scars in the liver will continue to build and replace healthy tissue. Gradually, the scars snake out farther, covering more of the healthy liver and grow together, or bridge, creating septa or bands of scar tissue. Fibrosis also restricts blood flow. When doctors want to determine how severe the scarring is, they examine the impact on the portal blood flow. The portal vein brings all the blood from the intestines to the liver to be processed.
Fibrosis in mild to moderate stages often does not cause symptoms. Due to a lack of symptoms, many people live with liver damage, or fibrosis, without being diagnosed until they have symptoms of cirrhosis. Fibrosis can be reversed if detected early enough and the underlying liver disease that caused the development of fibrosis can be cured or treated. If fibrosis is left untreated, it can lead to cirrhosis and liver cancer. It is important to remember that the process of fibrosis progressing to cirrhosis happens over a long period of time. The time it takes for fibrosis to progress is different for every disease and every person. Not everyone who develops fibrosis will progress to cirrhosis. Not everyone who gets cirrhosis will get cancer.
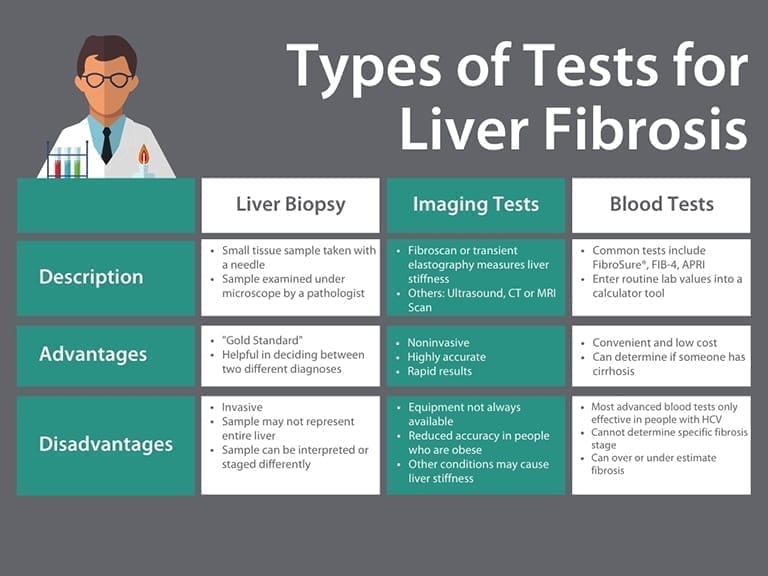
Testing Options
Until recently, liver biopsy was the only way doctors could determine the stage and degree of liver damage. Today, there are both blood and imaging tests that can determine liver damage. This is a brief overview of different types of tests your doctor may discuss with you.
Understanding Liver Biopsy Results
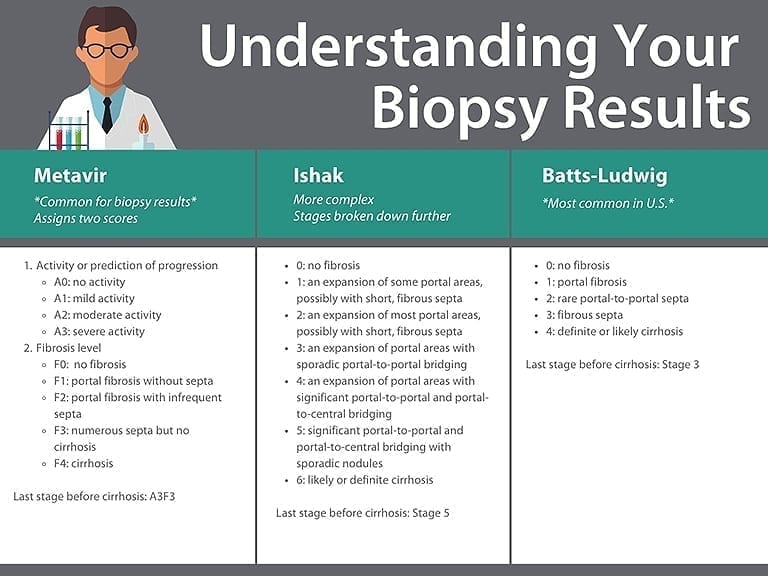
Understanding the results of these different tests can be a challenge. Healthcare providers use different scales to define the stages of liver damage. Different scales are used when a biopsy is done versus an imaging test, like a FibroScan®.
Common scales used to grade a liver biopsy are explained here. Most scoring systems examine the impact of fibrosis on the portal vein (which brings blood from the intestines) and the location and number of septa (connecting bands of scars).
If you have cirrhosis or are in the final stage before cirrhosis, please speak with your doctor about liver cancer screenings.
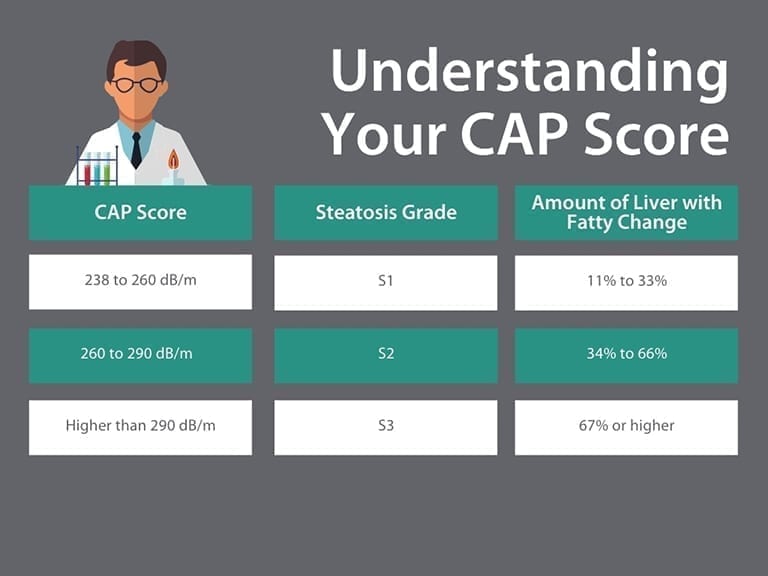
A FibroScan® is a special ultrasound for your liver. This imaging test is not invasive. By measuring the stiffness of the liver your doctor can detect both scarring and fatty change in the liver. Here, we have explained the information you may receive from your doctor if you have a FibroScan®.
Your CAP score is a measurement of fatty change in your liver. Fatty change (steatosis) is when fat builds up in your liver cells. This fat can impact your liver’s ability to function. Your doctor will use your CAP score to grade how much fatty change has happened in the liver. A CAP score is measured in decibels per meter (dB/m) and ranges from 100 to 400 dB/m. The table here shows ranges of CAP scores, the matching steatosis grade, and the amount of liver with fatty change.
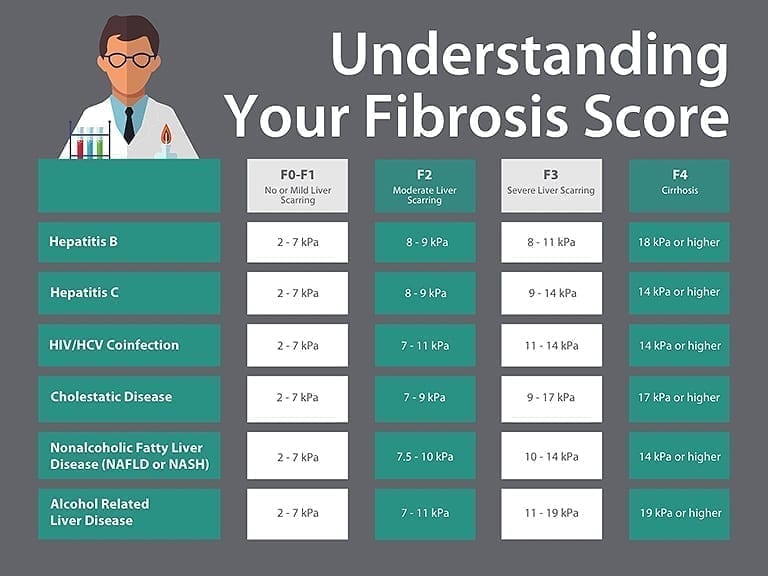
Reliability of Test Scores
This table shows liver diseases, ranges of fibrosis results, and the matching fibrosis score. The ranges of fibrosis results in the table are estimates. Your actual fibrosis score may not match the fibrosis score in the table. If you have more than one liver disease you may not be able to use this table. Your fibrosis result may be overestimated if you have liver inflammation caused by recent illness or drinking alcohol, benign or cancerous tumors in your liver, or liver congestion (when liver is too full of blood or other fluids). Your FibroScan® results may also be less accurate if you are obese, have ascites, or have too little bile flowing out of the liver.
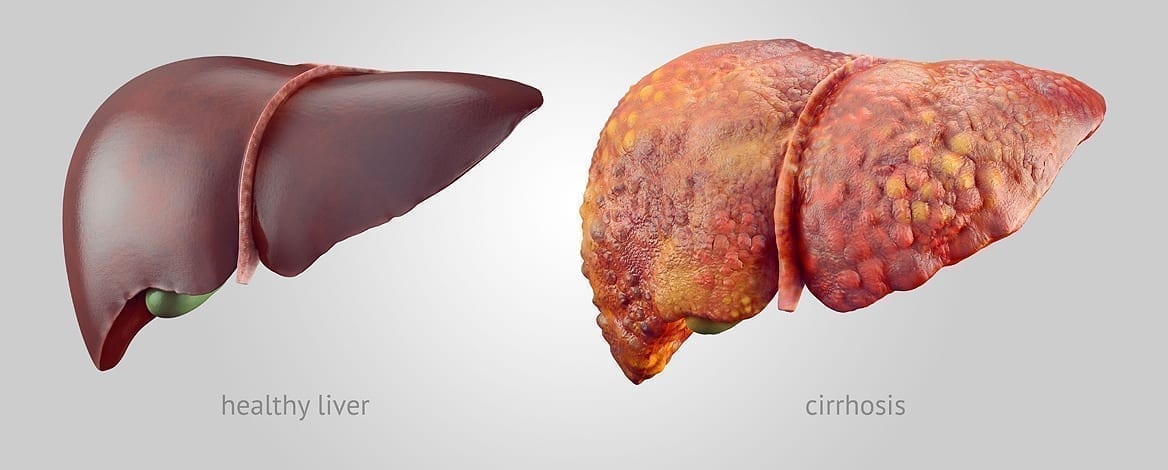
The final stage of fibrosis is cirrhosis…
Cirrhosis is where your liver is severely scarred and permanently damaged. While the word cirrhosis is most commonly heard when people discuss alcohol-induced liver disease, cirrhosis is caused by many forms of liver disease.
While fibrosis is reversible there is a point where the damage becomes too great and the liver cannot repair itself. There is no treatment that can cure cirrhosis. If possible, treating the underlying cause of cirrhosis may keep your cirrhosis from getting worse and help prevent liver failure. Successful treatment may slowly improve some of your liver scarring. It is important to avoid things that could damage your liver further like alcohol, certain medications and fatty food. Treatment for someone with cirrhosis often means managing the symptoms of cirrhosis and preventing further damage to avoid liver failure. Doctors treat liver failure with a liver transplant. Someone with cirrhosis is at a very high risk of developing liver cancer. It is very important to receive routine liver cancer surveillance if you have cirrhosis; most people who develop liver cancer have evidence of cirrhosis. Doctors also treat liver cancer with a transplant. It is important to note, people often live with cirrhosis for a long time before the option of liver transplant is discussed.
There is a big difference between liver functioning and disease progression. Our livers are resilient, continuing to function even when they become severely scarred. Because of this, some people may not experience symptoms or have elevated liver enzyme tests even though their liver is damaged. It is important to talk to your doctor about your risks for liver disease so you can receive imaging tests that may help diagnosis liver damage.
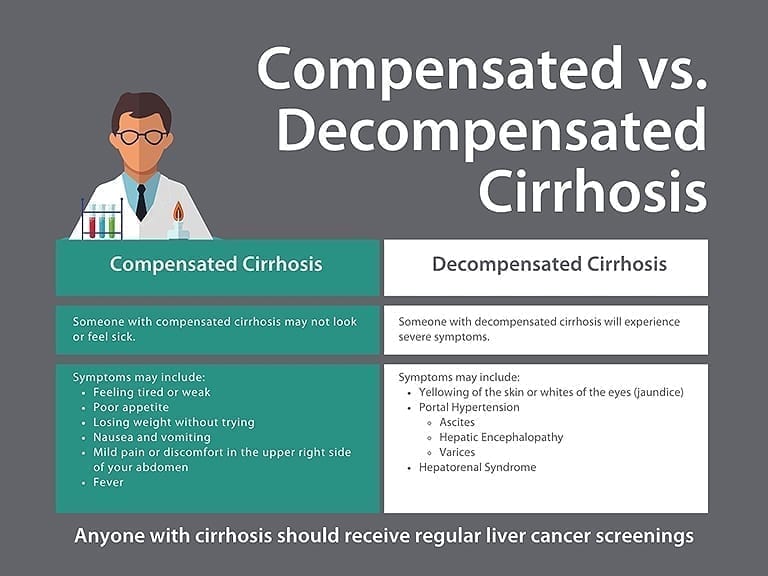
Compensated Cirrhosis v. Decompensated Cirrhosis
Cirrhosis is often categorized as either compensated or decompensated. Someone with compensated cirrhosis doesn’t necessarily look or feel sick. Their symptoms of the disease may be mild or nonexistent even though the liver is severely scarred. Someone with decompensated cirrhosis will feel and appear sick as their liver is struggling to function.
When someone has cirrhosis their liver shrinks and becomes hard, greatly impacting the liver’s ability to process the massive amounts of blood for which it’s responsible. The liver has two sources that supply blood to the liver – the hepatic artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood into the liver. Blood coming from our digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
When someone has decompensated cirrhosis the scar tissue blocks the blood meant to flow through the portal vein causing an increase of pressure known as portal hypertension. The blood carried in the portal vein is filled with proteins, toxins and other “stuff” meant to be filtered by the liver. The blood unable to enter the liver must find new routes; because the blood is not entering the liver, nutrients, toxins and more from the digestive system does not get properly filtered. Portal hypertension is responsible for symptoms like varices, ascites and encephalopathy. Hepatorenal syndrome can also occur when someone has decompensated cirrhosis.
Ascites
 The increased pressure of portal hypertension causes fluid to seep out and pool in the abdominal cavity. This is called ascites. When large amounts of fluid gather in the belly it can lead to swelling and pain and be very uncomfortable. Ascites can become infected, which can greatly impact the function of your kidneys, and can even be fatal.
The increased pressure of portal hypertension causes fluid to seep out and pool in the abdominal cavity. This is called ascites. When large amounts of fluid gather in the belly it can lead to swelling and pain and be very uncomfortable. Ascites can become infected, which can greatly impact the function of your kidneys, and can even be fatal.
Learn more about Ascites and how it’s managed by viewing our Ascites Information Page.
Learn more about Clinical Trial opportunities for Ascites patients.
Hepatic Encephalopathy
Ammonia is a waste product made when our body digests protein. The liver processes the ammonia, breaks it down to something called urea, and sends it to our kidneys to be released in urine. When someone has cirrhosis, ammonia is not eliminated, builds up, travels to the brain, and causes confusion, disorientation, coma, and even death. This is hepatic encephalopathy. Hepatic Encephalopathy (or HE) can be managed with medications that are taken regularly. One of these medications tries to eliminate extra ammonia through increasing the number of bowel movements. The other common medication is a powerful antibiotic which eliminates the bacteria in your digestive system responsible for creating the ammonia.
Learn more about hepatic encephalopathy in our HE Resource Center.
Learn more about clinical trial opportunities for HE patients.
Hepatorenal Syndrome
The liver is the largest filter in the body but works closely with our kidneys to eliminate waste from our bodies. When someone has cirrhosis, they may develop a serious complication where their kidneys begin to progressively fail. This is called hepatorenal syndrome.
Learn more about hepatorenal syndrome in our HRS Resource Center.
Jaundice
Our red blood cells have a substance in them called hemoglobin which is responsible for carrying oxygen. Bilirubin is a yellow chemical found in hemoglobin. Your body builds new cells to replace broken down red blood cells and the old ones are processed in the liver. The breakdown of the old cells releases bilirubin. A healthy liver processes bilirubin out of the body. If the liver cannot successfully do this function, bilirubin builds up in the body and your skin or the whites or your eyes may look yellow. This is called jaundice.
 This buildup of bilirubin can also cause someone’s urine to become very dark or their poop to be pale in color. Excess bilirubin is excreted in urine which causes someone’s pee to look very dark and brown, almost like a cola soda. The lack of bilirubin entering the gut causes someone’s stool to be very light in color. Jaundice does not only occur in people with cirrhosis. Many healthy babies have jaundice during the first week of life. Jaundice can also be due to blood diseases, genetic conditions, blockages of bile ducts, infections (like hepatitis A), and even some medications.
This buildup of bilirubin can also cause someone’s urine to become very dark or their poop to be pale in color. Excess bilirubin is excreted in urine which causes someone’s pee to look very dark and brown, almost like a cola soda. The lack of bilirubin entering the gut causes someone’s stool to be very light in color. Jaundice does not only occur in people with cirrhosis. Many healthy babies have jaundice during the first week of life. Jaundice can also be due to blood diseases, genetic conditions, blockages of bile ducts, infections (like hepatitis A), and even some medications.
Varices
When blood cannot flow through the portal vein into the liver it is forced to find new pathways, such as through the veins in the stomach and esophagus. These enlarged veins are called varices. These small veins are not meant to carry so much blood. When overloaded with blood, these veins can balloon, leak blood or even rupture, causing life-threatening bleeding. Varices usually don’t cause any symptoms unless they bleed. Signs of bleeding varices include:
- Vomiting large amounts of blood
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness (in severe cases)
Doctors can view these varices by inserting an endoscope (a thin flexible tube) through your mouth, down to your esophagus and stomach. Endoscopies are very important to avoid varices from bursting and bleeding. Doctors use endoscopies to check on the varices and, if needed, band them, or tie them off, to strangle the vein and keep them from bursting.
Liver cancer is cancer that begins in the cells of your liver. While several types of cancer can form in the liver, the most common type of liver cancer is hepatocellular carcinoma, or HCC, which begins in the main type of liver cells (hepatocytes). Liver cancer is one of the leading causes of cancer-related deaths worldwide. Over the last 30 years, rates of liver cancer have tripled in the United States. While most other common cancers have seen improved survival rates during this time period, liver cancer death rates have doubled.
It is very rare to develop HCC without first having cirrhosis. Because of this, when someone has been diagnosed with advanced fibrosis (F3) or cirrhosis they should receive regular surveillance for liver cancer. Finding and diagnosing liver cancer as soon as possible is essential. Early detection offers more potentially curative options, like resection (where the cancer and surrounding liver tissue is removed) and transplant.
Liver transplantation is a surgical procedure performed to remove a diseased or injured liver from one person and replace it with a whole or a portion of a healthy liver from another person, called the donor.
Since the liver is the only organ in the body able to regenerate, or grow back, a transplanted segment of a liver can grow to normal size within a few months. Often, transplanted livers are from people who were registered donors who passed away. Since the liver has such regenerative ability, however, it is possible for a living person to donate a portion of his or her liver to someone in need of a transplant.
To learn more about Liver Transplantation, click here.
To learn more about living donor liver transplantation, please visit our new Living Donor Liver Transplantation Information Center.
The best thing anyone can do for their health is to stay engaged in their healthcare. Be an active member of your care team by regularly visiting your healthcare provider, undergoing routine surveillance when needed, making the most of your appointments by asking questions and learning more about your health.
When possible, provide your doctor a detailed family health history to determine your own risks for liver disease. There are genetic or hereditary liver diseases that can run in families. Sometimes our genes put us at a greater risk for developing lifestyle related liver disease like Nonalcoholic Fatty Liver Disease and Alcohol Related Liver Disease. Your family members’ medical histories can be a useful piece of the puzzle when working with your doctor to resolve your own health concerns.
Being honest with our healthcare provider about your lifestyle is another important factor in determining risk for liver disease. Because your liver processes everything you eat, drink, breath, or absorb through our skin, it can be impacted by many different factors. It’s important to keep an updated list of the medications you take, even if it’s something you buy without a prescription at a store (diet supplements, vitamins, pain relievers, allergy medications, etc.). Be sure your doctor knows how often you take each type of medication and review medications that may have been prescribed by another healthcare provider. It is best to ask your healthcare provider before you begin taking any medications to be sure you are making the best choice for your health. Many medications can cause damage to the liver. Being open with your healthcare provider about your diet, exercise, and other lifestyle habits is very important! Your doctor can provide you the best care when they are aware of all the factors contributing to your health.
Progression of Liver Disease: 10 Questions about Progression Liver Disease
Progression of Liver Disease: 8 Questions about Hepatic Encephalopathy
Progression of Liver Disease Webcast Series: Cirrhosis and Signs of Liver Failure
Progression of Liver Disease Webcast Series: Stages of Liver Disease
Progression of Liver Disease Webcast Series: Liver Function and Liver Disease
Progression of Liver Disease
Last Updated on April 7, 2022
Share this page