Liver Awareness Month: Cirrhosis
Let’s Stop the Progression of Liver Disease
Did you have a chance to read our blog post about fibrosis and how liver disease is staged? If not, check it out here.
As a reminder, fibrosis is the process of scar tissue building up in the liver, replacing healthy functioning cells, and causing stiffening or hardening of the liver which reduces blood flow. The final stage of fibrosis is cirrhosis. Cirrhosis is where your liver is severely scarred and permanently damaged. While the word cirrhosis is most commonly heard when people discuss alcohol-induced liver disease, cirrhosis is caused by many forms of liver disease.
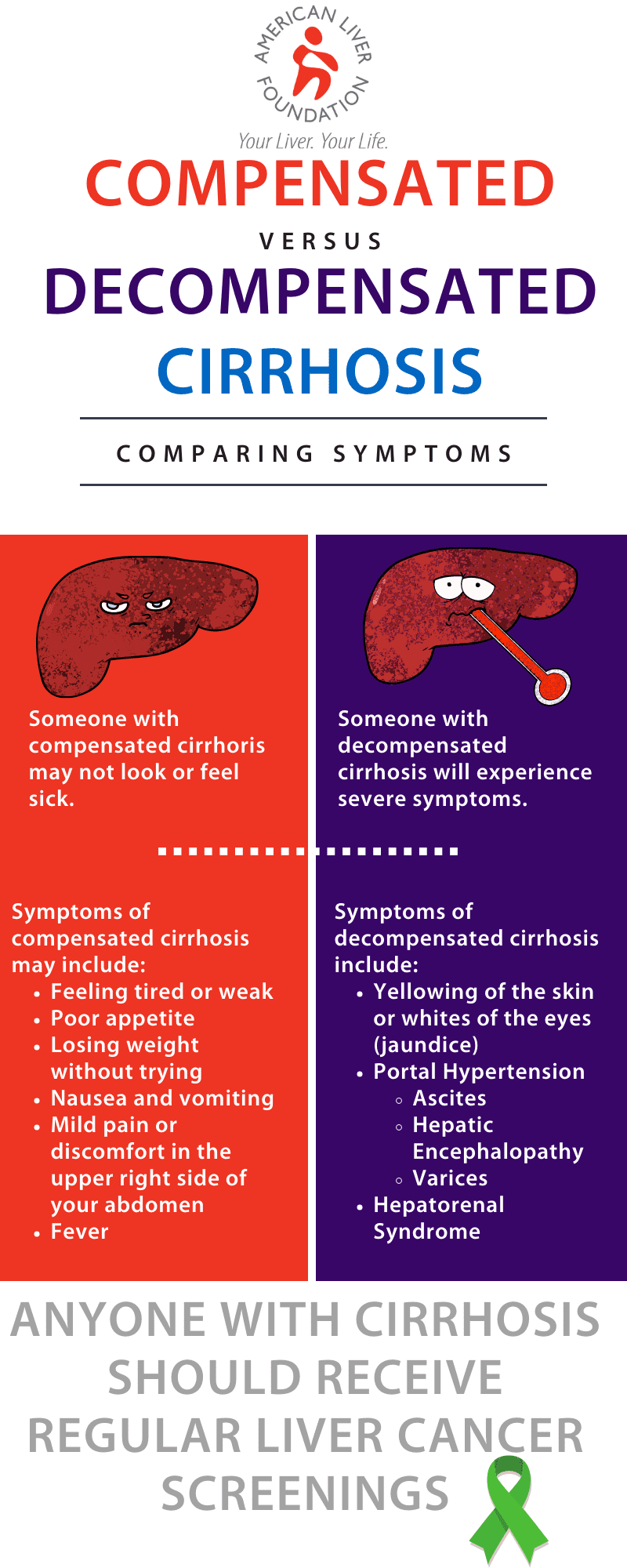
While fibrosis is reversible there is a point where the damage becomes too great and the liver cannot repair itself. There is no treatment that can cure cirrhosis. If possible, treating the underlying cause of cirrhosis may keep your cirrhosis from getting worse and help prevent liver failure. Successful treatment may slowly improve some of your liver scarring. It is important to avoid things that could damage your liver further, like alcohol, certain medications, and fatty food. Treatment for someone with cirrhosis often means managing the symptoms of cirrhosis and preventing further damage to avoid liver failure. Doctors treat liver failure with a liver transplant. Someone with cirrhosis is at a very high risk of developing liver cancer. It is very important to receive routine liver cancer surveillance if you have cirrhosis; most people who develop liver cancer have evidence of cirrhosis. Doctors also treat liver cancer with a transplant. It is important to note, people often live with cirrhosis for a long time before the option of liver transplant is discussed.
When we talk about cirrhosis, it’s important to remember that there is a big difference between liver functioning and disease progression. Our livers are resilient, continuing to function even when they become severely scarred; because of this, some people may not experience symptoms or have elevated liver enzyme tests even though their liver is damaged. It is important to talk to your doctor about your risks for liver disease so you can receive imaging tests that may help diagnosis liver damage.
Cirrhosis is often categorized as either compensated or decompensated. Someone with compensated cirrhosis doesn’t necessarily look or feel sick; their symptoms of the disease may be mild or nonexistent even though the liver is severely scarred. Someone with decompensated cirrhosis will feel and appear sick as their liver is struggling to function.
When someone has cirrhosis, their liver shrinks and becomes hard, greatly impacting the liver’s ability to process the massive amounts of blood for which it’s responsible. Did you know the liver’s biggest role is to filter our blood all day, every day? At any given moment, your liver contains about a pint, or 13% the body’s total blood supply; the liver filters more than a liter of blood every minute which is about 22 gallons of blood per hour and more than 250 gallons of blood in a 24-hour time period. There are two sources that supply all this blood to the liver: the hepatic artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood into the liver. Blood coming from our digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
When someone has decompensated cirrhosis the scar tissue blocks the blood meant to flow through the portal vein, causing an increase of pressure known as portal hypertension. The blood carried in the portal vein is filled with proteins, toxins, and other “stuff” meant to be filtered by the liver. The blood unable to enter the liver must find new routes; because the blood is not entering the liver, nutrients, toxins and other stuff from the digestive system does not get properly filtered. Portal hypertension is responsible for symptoms like varices, ascites, and encephalopathy. Hepatorenal syndrome can also occur when someone has decompensated cirrhosis.
When blood cannot flow through the portal vein into the liver it is forced to find new pathways, such as through the veins in the stomach and esophagus. These enlarged veins are called varices. These small veins are not meant to carry so much blood so they can balloon out, leak blood, or even rupture, causing life-threatening bleeding. Varices usually don’t cause any symptoms unless they bleed. Signs of bleeding varices include:
- Vomiting large amounts of blood
- Black, tarry, or bloody stools
- Lightheadedness
- Loss of consciousness (in severe cases)
Doctors can view these varices by inserting an endoscope (a thin flexible tube) through your mouth, down to your esophagus and stomach. If needed, the doctor will band them, or tie them off, to strangle the vein and keep them from bursting.
The increased pressure of portal hypertension causes fluid to seep out and pool in the abdominal cavity. This is called ascites. People with liver disease may experience different amounts of fluid building up—a little buildup of fluid may not cause any symptoms but as the amount of fluid increases it can cause waist size to expand and weight gain. When large amounts of fluid gather in the belly it can lead to swelling and pain and be very uncomfortable. The belly becomes hard from the fluid buildup, may resemble a pregnancy belly, and the belly button can become pushed out. Some people with ascites may develop swollen legs and ankles, called edema. Ascites can become infected for no reason which is called spontaneous bacterial peritonitis. This infection needs to be treated early with the right antibiotics; if left untreated the infection can be fatal. Someone with spontaneous bacterial peritonitis will usually feel even more uncomfortable and experience tenderness in their abdomen; they may develop a fever.
Ascites is treated with a low-sodium diet, medications called diuretics, removing the fluid, or surgery to reroute blood flow. Reducing sodium, or salt, is a first line therapy for ascites. If you have ascites, be sure to learn more from a nutritionist who specializes in the liver about your unique needs. Medications called diuretics may be prescribed which make the kidneys excrete more sodium and water into your urine, causing you to pee more frequently. Sometimes, diuretics are not enough, and the fluid will continue to build up. When this happens, someone may have a procedure called therapeutic paracentesis. During paracentesis, a doctor, usually an interventional radiologist, uses ultrasound to guide a needle into the abdomen and drain the fluid out of the body. The fluid will build back up and the procedure will need to be repeated. If someone continues to have fluid build-up or other treatments do not work, a doctor may consider a TIPS procedure (transjuglar intrahepatic portosystemic shunt). During a TIPS procedure, a new pathway is made to connect the portal vein, or one of its branches, with a vein in general circulation, bypassing the liver. While this shunt placement can improve ascites, it can also cause a worsening in hepatic encephalopathy or in liver function.
Ammonia is a waste product made when our body digests protein. The liver processes the ammonia, breaks it down to something called urea, and sends it to our kidneys to be released in urine. When someone has cirrhosis, ammonia is not eliminated, builds up, travels to the brain, and causes confusion, disorientation, coma, and even death. This is hepatic encephalopathy.
Learn more about hepatic encephalopathy in our HE Resource Center.
The liver is the largest filter in the body but works closely with our kidneys to eliminate waste from our bodies. When someone has cirrhosis, they may develop a serious complication where their kidneys begin to progressively fail. This is called hepatorenal syndrome.
Learn more about hepatorenal syndrome in our HRS Resource Center.
Our red blood cells have a substance in them called hemoglobin which is responsible for carrying oxygen; bilirubin is a yellow chemical found in hemoglobin. Your body builds new cells to replace broken down red blood cells and the old ones are processed in the liver. The breakdown of the old cells releases bilirubin. A healthy liver process bilirubin out of the body. If the liver cannot successfully do this function, bilirubin builds up in the body and your skin or the whites or your eyes may look yellow. This is jaundice.
This buildup of bilirubin can also cause someone’s urine to become very dark or their poop to be pale in color. Excess bilirubin is excreted in urine which causes someone’s pee to look very dark and brown, almost like a cola soda. The lack of bilirubin entering the gut causes someone’s stool to be very light in color. Jaundice does not only occur in people with cirrhosis. Many healthy babies have jaundice during the first week of life. Jaundice can also be due to blood diseases, genetic conditions, blockages of bile ducts, infections (like hepatitis A), and even some medications.
American Liver Foundation is solely responsible for this content, which is made possible through generous support from Mallinckrodt and Salix.
Last Updated on November 11, 2021
Share this page